Standardized guidelines can help radiologists navigate the legal landscape of imaging pregnant women with ionizing radiation, according to a July 15 editorial published in the Journal of the American College of Radiology (ACR).
A team led by Katherine Frederick-Dyer, MD, from Vanderbilt University Medical Center in Nashville, TN highlighted an updated practice parameter co-developed by the American College of Radiology (ACR) and the Society for Pediatric Radiology (SPR). The parameter provides best practices for imaging pregnant women or women who can become pregnant.
“Importantly, it’s an updated guideline and an evolving document that will continue to reflect new information in best practices as things change and develop, new risks are identified, and old risks are set aside,” Frederick-Dyer told AuntMinnie.com.
Since the overturning of Roe v. Wade with the 2022 U.S. Supreme Court ruling on Dobbs v. Jackson Women's Health Organization, medical professionals have had to adjust their practices to reflect ever-changing state-level policies pertaining to fetal health services. For radiologists, this includes navigating how best to image pregnant women or women who may not know if they’re pregnant but decline testing.
The editorial authors wrote that differing abortion restrictions by state could be confusing for both patients and radiologists, and women may decline pregnancy testing out of concern for the legal implications of an established pregnancy.
The authors highlighted that this indicates the need for a standard, evidence-based approach to determine when pregnancy testing should be recommended. This includes how to best inform patients with an established pregnancy of imaging exam risks.
The ACR and SPR in 2023 updated their practice parameter for this area of imaging. Some points made in the parameter include the following:
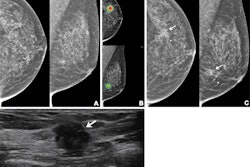
- Very low-dose imaging exams such as mammography and radiography, excluding imaging of the abdomen and pelvis, do not require pregnancy verification. The same goes for CT imaging outside the abdomen and the pelvic/hip area.
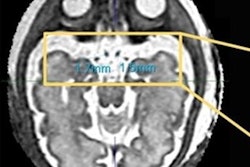
- Pregnancy status should be verified prior to imaging that includes the abdomen and pelvis in the field of view, such as fluoroscopy, CT, and radiography.
- Radiopharmaceutical agents such as technetium-99m (Tc99m)-sulfur colloid and F-18 FDG with very short half-lives (resulting in very low-dose radiation exposure) pose minimal risk. When using agents with a short half-life, a patient's medical history showing they cannot become pregnant should be adequate without additional pregnancy testing.
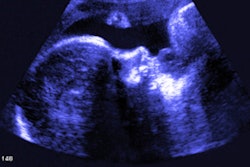
- Once a pregnancy is established, a radiologist should consider whether the exam is needed or can be delayed until after delivery, if there are alternative exams available (ultrasound or MRI), and if changes can be made to protocols to decrease radiation dose.
Additionally, the practice parameter notes that every exam should be performed with the patient’s consent and provides model language to convey information in a positive light.
Frederick-Dyer said that in the future, she would like to see more information in guidelines about dealing with theranostics agents and their potential risks on fetuses.
“Just because they’re a woman who’s pregnancy-capable doesn’t mean they should receive a lesser standard of care,” she said. “They should at least receive the standard of care and assistance for navigating these particular situations.”
She also credited the American Association for Women in Radiology for the editorial, with whom she and colleagues collaborated.
The full editorial can be found here.