Some factors tied to first breast cancers can have a negative impact on screening mammography's ability to find future cancers, according to research published October 5 in Clinical Imaging.
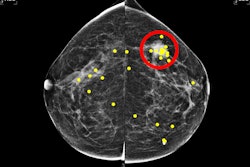
A team led by Julie Hamzah, MBBS, from Singapore General Hospital, found that symptomatic first breast cancers, dense breasts, and the presence of trabecular thickening on mammography are tied to mammogram detection failure of ipsilateral second breast cancers. Also, mammogram-occult primary breast cancer is the most important risk factor for a contralateral mammogram-occult second breast cancer, the team found.
“A personalized surveillance program employing a supplemental imaging modality adjunct to mammography may be considered for this select group of breast cancer survivors,” Hamzah and colleagues wrote.
Women with a personal history of breast cancer are at elevated risk of developing future breast cancers. Surveillance imaging strategies are employed to help closely monitor the possible development of these cancers.
However, varying factors can impact the performance of mammography. These include breast density, tumor type, and mammographic characteristics mistaken to be benign post-treatment changes in the treated breast among others.
Hamzah and co-authors sought to determine factors that can predict poorer second breast cancer detection on mammography of the ipsilateral and contralateral breast separately.
The study included data collected between 2006 and 2017 from 274 second breast cancer cases diagnosed within 10 years of first breast cancer cases. Of these, 39.4% (n = 108) were ipsilateral second cancers and 60.6% (n = 166) were contralateral.
The researchers observed that 35 (32.4%) of the ipsilateral second cancers and 42 (25.3%) of the contralateral second cancers were mammogram-occult, respectively (p = 0.218).
Using multivariate analysis, the team also found significant associations between mammogram-occult ipsilateral second breast cancers: symptomatic first breast cancer (p = 0.041), prevailing dense breast tissue at the time of second breast cancer diagnosis (p = 0.003), and trabecular thickening on surveillance mammograms (p = 0.017).
Finally, the investigators observed that mammogram-occult first breast cancer was the only factor significantly tied to mammogram-occult contralateral second breast cancer (p < 0.001).
The study authors highlighted that their findings could inform additional guidance in the planning of a personalized surveillance program using adjunct imaging, including MRI, ultrasound, and digital breast tomosynthesis (DBT). They added that future studies should evaluate factors that affect the performance of DBT in surveillance imaging.
“The utility of this imaging-based study should, therefore, be viewed in the clinical context of part of a wider risk-based model of breast cancer surveillance approach,” they concluded.
The study can be found in its entirety here.