Automated breast ultrasound (ABUS) with remote reading may improve access to breast cancer screening and early detection in low-resource settings, suggest findings published October 23 in the American Journal of Roentgenology.
Researchers led by Hongping Song, MD, PhD, from Xijing Hospital, Fourth Military Medical University in China found that ABUS screening with remote reading achieved benchmark performance metrics for cancer detection when compared to mammography, with infrequent interval cancers.
“Screening by ABUS may help to address challenges in national mammography screening in China related to cost, equipment installation, implementation, and low adoption rates,” Song and colleagues wrote.
Radiology researchers in recent years have explored the potential of ABUS screening in improving breast cancer detection and point-of-care technologies to improve access to screening. Song and co-authors noted that Chinese women have faced barriers to implementing a population-based mammographic screening program.
The researchers evaluated the performance of ABUS with remote reading as the primary screening modality for breast cancer in a prospective study.
The study included 5,978 enrolled asymptomatic women ages 35 to 69 years. The women attended screenings at 46 community health centers across 18 Chinese provinces in 2021. They underwent screening ABUS as the sole breast cancer screening modality, with images acquired by a technologist at a community health center.
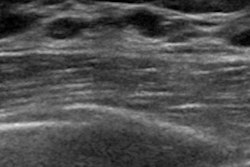
 Axial (A) and coronal (B) ABUS images of the right breast show 4-mm irregular hypoechoic mass (arrows) at the 11-o’clock position. The background echotexture is heterogeneous. The mass was assessed as BI-RADS category 4. The patient underwent biopsy at a local hospital and subsequent surgical excision. Surgical histopathologic assessment revealed a 6-mm grade 2 invasive ductal carcinoma without axillary lymph node metastasis; the cancer was estrogen receptor positive, progesterone receptor positive, and HER2 negative. The case is consistent with cancer detected by ABUS screening.ARRS
Axial (A) and coronal (B) ABUS images of the right breast show 4-mm irregular hypoechoic mass (arrows) at the 11-o’clock position. The background echotexture is heterogeneous. The mass was assessed as BI-RADS category 4. The patient underwent biopsy at a local hospital and subsequent surgical excision. Surgical histopathologic assessment revealed a 6-mm grade 2 invasive ductal carcinoma without axillary lymph node metastasis; the cancer was estrogen receptor positive, progesterone receptor positive, and HER2 negative. The case is consistent with cancer detected by ABUS screening.ARRS
The 3D volumetric data were transferred via cloud-based software to a single remote reading center, where two breast radiologists independently interpreted batches of images using BI-RADS. Meanwhile, a third radiologist at the remote reader center resolved discrepancies.
The team returned diagnostic reports to the community centers and patients sought follow-up care at local hospitals.
ABUS detected 24 cancers from the dataset and helped to diagnose two interval cancers. ABUS achieved a cancer detection rate of four per 1,000 women, with an abnormal interpretation rate of 11.9%.
The researchers also noted that 95.8% (N = 23) of ABUS-detected cancers were invasive. These had a median diameter of 10 mm. Of the invasive cancers, 17 (73.9%) were node-negative.
Finally, ABUS achieved a sensitivity rate of 92.3%, a specificity rate of 88.4%, a biopsy rate of 1.7%, and a positive predictive value (PPV) of biopsy of 24%.
The study authors highlighted that their results show ABUS’ potential when combined with teleradiology to improve breast cancer screening access in resource-limited areas or areas without mammography access.
“This approach could be integrated into radiology departments’ workflow to provide high-quality breast ultrasound services to remote areas lacking subspecialized breast radiologists,” they wrote.
Still, they cautioned that to ensure patient privacy and accurate results, teleradiology must be implemented with attention to data security, quality assurance, and compliance with healthcare regulations.
The full study can be found here.