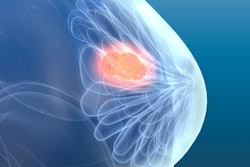
Starting breast cancer screening at age 40 is tied to improved patient outcomes and reduced healthcare spending on treatment, according to research published January 2 in JAMA Network Open.
A team led by Anna Wilkinson, MD, from the University of Ottawa in Ontario, Canada, found that while screening costs increased due to the number of lifetime screens, they were offset by reduced breast cancer therapy costs. It also highlighted digital mammography as a cost-effective tool in reducing breast cancer mortality.
“These results have important policy implications for all single-payer health systems and call for greater investment in screening programs,” the Wilkinson team wrote.
New breast cancer detection and treatment methods continue to make their way into the clinic and improve patient outcomes. However, the researchers pointed out that it’s not known how the cost-effectiveness of screening mammography is potentially linked to treatment costs.
Wilkinson and colleagues sought to determine the cost-effectiveness of population-based breast cancer screening with current treatment standards in mind. They used the Canadian Partnership Against Cancer/Statistics Canada OncoSim-Breast microsimulation model to estimate the impact of various screening schedules on clinical outcomes and treatment costs.
The team-based breast cancer treatment costs on activity-based costing published in 2023, specific to a publicly funded health system in Ontario, Canada. It also modeled five screening scenarios based on age and time between screenings. These included the following: no screening, biennial (ages 50 to 74 and 40 to 74), hybrid (biennial ages 40 to 49 and annual ages 50 to 74), and annual screening (ages 40 to 74).
The researchers found that starting breast cancer screening at age 40 rather than age 50 was tied to improved outcomes. These included the number of deaths averted, life-years saved, and quality-adjusted life years (QALY) gained. Beginning screening at age 40 also led to reduced spending on breast cancer treatment, the researchers reported.
Incremental cost-effectiveness ratios for biennial screening at ages 40 to 74 saved on costs compared with biennial screening at ages 50 to 74. This included 49,759 Canadian dollars ($34,462 U.S.) saved per death averted, 1,558 Canadian dollars ($1,079 U.S.) per life years saved, and 2,007 Canadian dollars ($1,390) saved per QALY gained.
The group found that annual screening at ages 40 to 74 led to more cost-effectiveness while achieving the best breast cancer outcomes compared with the current Canadian standard of biennial screening at ages 50 to 74. This included costs of 25,501 Canadian dollars ($17,662 U.S.) per death averted, 1,100 Canadian dollars ($762 U.S.) per life year saved, and 1,447 Canadian dollars ($1,002 U.S.) per QALY gained.
With these results in mind, screening mammography can simultaneously improve clinical outcomes and reduce healthcare costs, according to the investigators.
“This work highlights the importance of public health and funders regularly assessing updated cost-effectiveness when evaluating the risks and benefits of population-based screening programs,” they noted.
The authors added that cancer management costs will likely continue to increase, making earlier diagnosis all the more important to keep treatment costs down.
“Organized breast cancer screening programs enable earlier detection of breast cancer, improving clinical outcomes while simultaneously minimizing treatment burden and costs, thereby improving health equity,” they wrote.
The full study can be found here.