Contrast-enhanced conebeam breast CT (CBBCT) imaging features can help identify lymphovascular invasion (LVI) status in breast cancer patients, a study published February 13 in Academic Radiology found.
A team led by Zhaoxiang Ye, MD, PhD, from the National Clinical Research Center for Cancer in Tianjin, China, found that LVI was tied to various CT imaging features, including histologic type, Ki-67 index, and increased ipsilateral whole-breast vascularity (IIV) number and degree, among others.
“Our study suggests that CBBCT imaging features … can serve as biomarkers for predicting LVI in breast cancer patients, which helps clinicians make personalized treatment decisions and ensures optimal prognosis for patients,” Ye and colleagues wrote.
LVI refers to the presence of malignant cells within lymphatic or blood vessels surrounding cancer tumors. Previous studies suggest that LVI is linked to negative prognosis, local recurrence, and distant metastases. And while assessing LVI relies on postoperative pathological diagnosis, the researchers noted that this has no value for preoperative assessment.
CBBCT in previous studies has shown advantages over supplemental breast MRI and ultrasound. The researchers highlighted the modality’s ability to assess breast calcifications and hemodynamic features at the same time. These studies also suggest that CBBCT could have value in breast cancer diagnosis, tumor size assessment, and molecular subtype prediction.
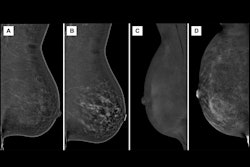
Ye and co-authors investigated potential ties between contrast-enhanced CBBCT imaging features and LVI status in breast cancer patients. The study included data collected between 2020 and 2023 from 401 women who underwent this imaging exam. Two radiologists reviewed the image features independently.
The team found that LVI status was significantly tied to the following features: histologic type, Ki-67 index, adjacent vessel sign (AVS), (IIV) number, and IIV degree (all p < 0.05). On multivariate logistic regression analysis, independent risk factors for LVI included AVS (odds ratio [OR] = 4.367, p < 0.001) and IIV degree (OR of moderate and prominent IIV = 4.732, 3.641, both p < 0.005).
For masses, LVI was associated with calcification, AVS, IIV number, and IIV degree (all p < 0.05). AVS and moderate-to-prominent IIV serve as independent predictors.
In nonmass enhancements, AVS, IIV number, and IIV degree were significantly tied to LVI (all p < 0.05). And for these enhancements, moderate-to-prominent IIV was an independent factor.
The team also developed a predictive model based on clinicopathological data and CBBCT imaging features. The model, which included AVS and IIV degree, achieved excellent performance, with an area under the curve (AUC) of 0.804.
With these results in mind, the researchers noted that evaluating IIV in breast cancer “could provide preliminary information on breast cancer microenvironment and predict LVI status.”
The study authors also highlighted that radiomics studies for LVI status based on CBBCT should be studied, writing that such data could aid in benign and malignant tumor differentiation, lymph node status, and metastatic burden identification.
The full study can be found here.