Breast texture patterns on mammography may be tied to elevated breast cancer risk in women with dense breasts, according to research published May 13 in Radiology.
A team led by Stacey Winham, PhD, from the Mayo Clinic in Rochester, MN, found six parenchymal phenotypes that showed significant association with invasive cancer risk in both Black and white women with dense breasts, which may also predict false-negative exams and interval cancer diagnosis.
“While our findings are not ready for the clinic, they underscore the importance of mammographic texture and complexity to breast cancer risk,” corresponding author Celine Vachon, PhD, told AuntMinnie.
As breast radiologists integrate breast density more into cancer risk assessment, research has shown that screening women with dense breasts is not a one-size-fits-all approach. Previous reports suggest that two women with the same breast density may show differences in their tissue patterns at mammography.
Previous studies have also characterized mammographic texture by extracting imaging features and assessing potential associations with higher cancer risk.
The Vachon team defined parenchymal phenotypes based on radiomic texture features from full-field digital mammography (FFDM). The group also evaluated potential associations between these phenotypes, future cancer risk and masking, and race and ethnicity.
The researchers employed a two-stage study design. This included a retrospective cross-sectional study of 30,000 randomly selected women with four-view FFDM and a nested case-control study of 1,055 women with invasive breast cancer. For the latter, this consisted of 151 Black women and 893 white women matched to 2,764 women without breast cancer (411 Black women and 2,345 white women) sampled from 2008 to 2019 from three different practices.
The team also extracted and standardized 390 radiomic features by using an automated pipeline, adjusting for age and practice.
Vachon and colleagues defined and replicated six clusters and six principal components that the group deemed to be linked to a higher risk of invasive breast cancer (p = 0.01 and p < 0.001, respectively). This was after adjustment for age, body mass index, and BI-RADS breast density.
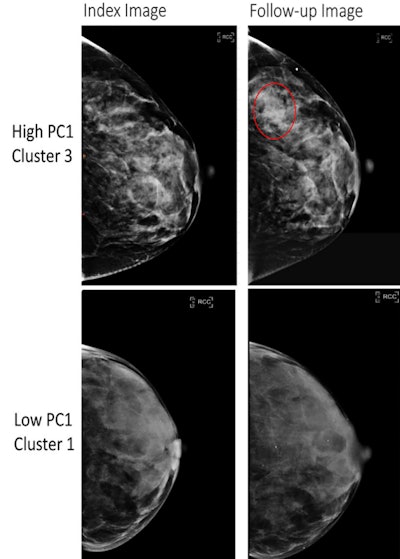 Full-field digital mammography (FFDM) images in a 52-year-old woman show a high-risk phenotype (top), and FFDM images in a 58-year-old woman show a low-risk phenotype (bottom). The high-risk phenotype was defined by having high values of the first principal component (PC1) and was assigned to cluster 3 (top row), and the low-risk phenotype was defined by having low values of the PC1 and was assigned to cluster 1 (bottom row). The index images (left side; before any diagnosis of cancer) are provided as well as follow-up images obtained at either the time of cancer diagnosis (for the high-risk phenotype, top right) or at the last follow-up (low-risk phenotype, bottom right). The red circle indicates the location of subsequent breast cancer. Both women had a BI-RADS breast density of C. The woman at high risk for breast cancer was Black and the woman at low risk for breast cancer was white.RSNA
Full-field digital mammography (FFDM) images in a 52-year-old woman show a high-risk phenotype (top), and FFDM images in a 58-year-old woman show a low-risk phenotype (bottom). The high-risk phenotype was defined by having high values of the first principal component (PC1) and was assigned to cluster 3 (top row), and the low-risk phenotype was defined by having low values of the PC1 and was assigned to cluster 1 (bottom row). The index images (left side; before any diagnosis of cancer) are provided as well as follow-up images obtained at either the time of cancer diagnosis (for the high-risk phenotype, top right) or at the last follow-up (low-risk phenotype, bottom right). The red circle indicates the location of subsequent breast cancer. Both women had a BI-RADS breast density of C. The woman at high risk for breast cancer was Black and the woman at low risk for breast cancer was white.RSNA
The principal components also showed similar associations among Black and white women (p = 0.23). And they were also positively associated with false-negative findings (p = 0.004) and symptomatic interval cancers (p = 0.006).
The researchers also reported that area under the curve (AUC) values increased for all breast cancer end points when incorporating the principal components.
Comparison of AUC values when including, excluding principal components from radiomics features | |||
Predictive measure | Without principal components | With principal components | p-value |
False-negative findings | 0.66 | 0.73 | 0.004 |
Symptomatic inverse cancers | 0.68 | 0.77 | 0.006 |
The study authors “expect these phenotypes to improve future risk prediction to better identify women at high risk for breast cancer for risk reduction strategies and tailored screening,” they wrote. They also suggested this approach to be used on low-risk women who may be able to extend screening intervals.
Vachon said that work is underway to “examine whether these parenchymal phenotypes add to known risk models for breast cancer, and in particular, risk of advanced breast cancer.”
“We will next characterize parenchymal phenotypes from screening digital breast tomosynthesis [DBT], which … provides superior visualization of tissue and reduced superimposition of tissue relative to 2D mammography,” she told AuntMinnie. “We hypothesize that 3D imaging in DBT may provide more accurate and predictive radiomic features, which will enhance breast cancer risk prediction.”
The results show the growing role of radiomic phenotypes for assessing breast cancer risk, according to an accompanying editorial written by Benoît Mesurolle, MD, from Pôle Santé République – Elsan in Clermont-Ferrand, France, and Mona El Khoury, MD, from the University of Montreal in Canada.
“Their results are convincing and promising, showing a reproducible tool able to predict the risk of invasive breast cancer and false-negative findings,” the duo wrote.
The editorial authors called for larger studies that include data from multiple races and ethnicities to reinforce their results.
The full study can be accessed here.