An AI tool could help find interval breast cancers earlier, suggest findings published October 28 in Radiology.
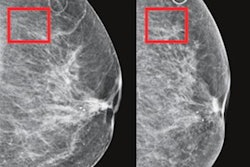
Further workup of mammograms within the top 20% of scores assigned to women by the Mirai risk model could result in over 40% of interval cancers being found, wrote a team led by Fiona Gilbert, MD, from the University of Cambridge in England.
“This has huge implications for radiologists,” Gilbert told AuntMinnie. “We actually think prediction tools like Mirai are better able to [prevent] women [from] having these larger interval cancers between screenings.”
Radiology researchers continue to explore the effectiveness and feasibility of risk modeling for breast cancer from deep-learning algorithms. One such algorithm, Mirai, has shown success in prior studies in predicting breast cancer from a single mammogram. Mirai has now been validated on about 2 million mammograms across 21 countries.
Gilbert and colleagues studied Mirai’s ability to identify women who developed interval cancers in the U.K. breast screening program. The program invites women aged 50 to 70 years for triennial mammography. The researchers highlighted that breast screening programs could be better employed by improving the selection criteria for women who could benefit from supplemental imaging.
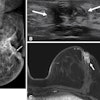
For the retrospective study, the researchers had Mirai process digital screening mammograms with negative results collected from a three-year cohort (2014 to 2016) across two sites and two primary mammography systems. They used no cancer diagnosis within 40 months of negative screening, confirmed histopathologically, as the reference standard.
The study included 134,217 exams from the same number of women, including 524 interval cancers.
Fiona Gilbert talks about how deep learning tools may help better predict women who need additional breast imaging tests.
The team found no evidence of performance differences among interval cancer predictions at one, two, and three years. This included area under the receiver operating characteristic curve (AUC) values of 0.72, 0.67, and 0.67, respectively (p ≥ 0.63). The same trend went across age quartiles, with concordance index (C Index) ranges of 0.67 to 0.71 (p ≥ 0.73), and across different breast densities (C index range, 0.67 to 0.7; p ≥ 0.99).
The researchers also reported no significant differences in performance when independently comparing AUCs for low (AUC, 0.65) and high (AUC, 0.66) densities only (p = 0.68) or for younger (AUC, 0.68) and older (AUC, 0.67) ages only (p = 0.90).
The team also had Mirai predict interval cancers for women assigned the highest 1%, 5%, 10%, and 20% of three-year risk scores. It found that Mirai predicted 3.6%, 14.5%, 26.1%, and 42.4% of interval cancers for these scores, respectively. Identifying the interval cancers is equivalent to an additional cancer detection rate of 0.1, 0.6, 1, and 1.7 per 1,000 exams.
Gilbert and Joshua Rothwell, a medical student at the University of Cambridge pursuing his PhD, said the team will next look at the types of cancer that Mirai can detect and compare Mirai with other prediction tools. They are also looking to conduct prospective studies using Mirai.
Joshua Rothwell discusses future research opportunities for Mirai in breast imaging.
In an accompanying editorial, Liane Philpotts, MD, from Yale University in New Haven, CT, wrote that the findings “are encouraging and offer a potentially important step toward tailored precision breast cancer screening for women.”
She also noted the current limitations of deep learning for predicting interval cancers, with the highest threshold used in the study not achieving 50% or higher.
“This humbling fact underscores the difficulty -- for both humans and machines -- of predicting and detecting breast cancers with mammography,” Philpotts wrote.
Read the entire study here.