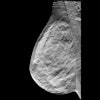
Handheld ultrasound (HHUS) has some advantages over automated breast ultrasound (ABUS) for second-look evaluation of MRI-detected breast lesions, suggest findings published January 23 in Academic Radiology.
HHUS showed similar performance to ABUS in terms of lesion detection based on lesion size, depth, lesion type, and localization among other features, wrote a group of researchers led by Ulku Tuba Parlakkilic, MD, from Acibadem Mehmet Ali Aydınlar University in Istanbul, Turkey. POCUS also achieved similar sensitivity compared with ABUS, though the latter showed higher positive predictive value (PPV).
“Our results show that the two methods are complementary to each other and have the potential to increase lesion detection rate when used together in clinics where both methods are available,” Parlakkilic and colleagues wrote.
Second-look breast ultrasound refers to the imaging of suspicious lesions first found on breast MRI. Its main purpose is to make way for ultrasound-guided needle biopsy. Second-look ultrasound could also provide more information for characterizing MRI-detected lesions.
No consensus exists on whether HHUS or ABUS should be used in this manner. Prior research suggests that ABUS is superior to HHUS in showing architectural distortion. But both modalities have similar cancer detection rates and can comparably differentiate benign from malignant lesions.
The Parlakkilic team compared the diagnostic performance of HHUS and ABUS as second-look ultrasound techniques in patients referred for MRI-guided breast biopsy.
The single-center prospective study included 54 women with 66 MRI-detected breast lesions referred for MRI-guided biopsy. All women underwent second-look evaluation with both HHUS and ABUS. Histopathology or imaging follow-up served as the reference standard. Women underwent ultrasound-guided biopsy or preoperative surgical localization if either ultrasound technique detected their lesions.
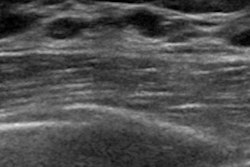
Of the total lesions, 30 were benign, 16 were high-risk, and 20 were malignant. HHUS detected 56 of the lesions (84.9%) while ABUS found 46 (69.7%, p = 0.01).
Two out of 13 lesions detected only by HHUS and two out of three (66.7%) lesions detected only by ABUS were malignant. None of the seven lesions that could not be detected by either method were malignant.
The team also reported no statistically significant difference between the number of lesions detected on HHUS and ABUS in terms of the following characteristics: lesion size, depth, lesion type (mass vs. nonmass), lesion localization, parenchymal density, kinetic features, or morphological findings (p > 0.05 for all).
Both techniques achieved a sensitivity of 90%. However, ABUS achieved a higher PPV over HHUS (39.1% vs. 32.1%). The team suggested that this was due to a higher proportion of malignant lesions among ABUS-only findings.
“However, we think that although a higher PPV is advantageous in the screening setting, it is not an advantage in the second-look ultrasound setting, because not finding a lesion with ABUS would lead to an MRI-guided biopsy,” the study authors wrote. “We cannot omit a biopsy due to a negative ABUS examination, as it can have false negative results.”
The authors also called for future research with larger cohorts to better understand ABUS’ capabilities. They suggested that combining ABUS with HHUS and the incorporation of AI could further improve second-look breast imaging.
“Moreover, we think that ABUS will and can be very helpful for radiologists with limited experience in second look US evaluation of the breast,” the authors wrote.
Read the full study here.