VIENNA - A series of studies at the 2002 European Congress of Radiology on Friday investigated the use of computer-aided detection (CAD) in breast screening programs. A common theme was that, while CAD can be a useful addition to a mammography practice, the verdict is still mixed as to whether it is advanced enough to replace second readings by an experienced radiologist.
All of the Friday presentations involved the use of the Second Look CAD system (CADx Medical Systems, Montreal, Canada). Second Look is one of two commonly used CAD systems, the other being the ImageChecker by R2 Technology of Los Altos, CA.
One of the potential questions facing mammographers is whether CAD could replace double reading of mammograms. Studies have demonstrated that double reading can reduce the number of missed breast cancers by up to 15%, but the practice is both costly and time intensive.
In the first presentation, Dr. Rachel Brem of George Washington University Medical Center, Washington, DC, presented data from a multicenter review that measured the performance of radiologists with and without CAD. The group studied 377 breast cancer cases from 18 participating centers. The cases consisted of patients who had normal screening mammograms 9-24 months before a cancer diagnosis was reached.
The 377 cases were reviewed by a panel of three blinded radiologists, selected from panel of six expert mammographers. Additional workup was recommended in 317 cases, and in 177 of these cases, the area for which workup was requested turned out to be the region that was subsequently diagnosed with breast cancer. The group termed these cases missed cancers, Brem said.
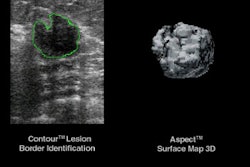
The cases were then evaluated by the Second Look system. The CAD unit analyzes digitized mammograms with software algorithms and highlights suspicious areas -- microcalcifications and masses -- with marks to flag them for further review by radiologists.
Brem’s group found that radiologists working without CAD had a sensitivity of 75.4%. Working with CAD, their sensitivity rose to 91.4%, an increase of 21.2%. This translates into 21,200 extra cancers detected for every 100,000 women diagnosed with cancer, according to Brem.
"CAD has demonstrated an increase in the sensitivity for breast cancer detection, and is a reasonable and viable alternative to second reading for the improved detection of breast cancer," she said.
In a second presentation from the same study, Dr. Janet Baum from Beth Israel Deaconess Medical Center in Boston discussed her group’s investigation of whether CAD increased the workup rate at locations where it’s being used. The study addressed the question of whether false positives detected by CAD prompt mammographers to order more follow-up studies to identify suspicious areas.
Ten radiologists from five sites reviewed 3,946 screening mammograms with and without CAD. They defined workup as anything requiring additional views, such as spot and magnification views, additional projections, or ultrasound.
The historical average workup rate of the radiologists involved in the study over the past year was 13.3%, Baum said. In this study, working without CAD, the radiologists had a prospective workup rate of 16.6%. With CAD, the workup rate rose to 17.2%, an increase of 0.5%, which Baum said was not statistically significant. In addition, CAD increased the total time spent reviewing cases by less than 10%, she said.
Another group, from the Institute of Diagnostic and Interventional Radiology at Friedrich Schiller University in Jena, Germany, investigated whether using CAD contributed to unnecessary follow-up procedures.
The researchers examined a group of 187 women with 748 images, with 40 histologically proven breast cancers, 49 histologically proven benign lesions, and 100 normal cases. Five blinded observers with no experience in CAD reviewed the cases, with and without CAD.
The group found that specificity actually improved with CAD, from 83% for those not using it to 86% for the group that used it, according to Dr. Christiane Marx, who presented the study. However, they also found that CAD had a statistically insignificant increase on sensitivity -- it only increased sensitivity from 78% to 78.5%. Marx said that training before using CAD in routine mammography is important, and may influence diagnostic quality.
CAD and lesion size and shape
Another study by the Friedrich Schiller team looked into whether the CAD system’s tumor detection rate was affected by the size and histopathology of lesions. The group retrospectively evaluated 214 consecutive cases with 220 biopsy-proven lesions.
The team discovered that CAD performed best when analyzing the most common lesion sizes and most prevalent types of cancer, according to Dr. Ansgar Malich, who presented the study. CAD had a sensitivity of 100% for lesions in the 10-30 mm range, and 88% for lesions smaller than 10 mm. The system’s sensitivity dropped, however, when examining larger lesions: it stood at 74% for lesions in the 31-40 mm range, and at 56% for lesions larger than 40 mm.
The system had the highest sensitivity when examining masses found to be invasive ductal carcinoma (IDC), with a 92% rating, and 85% for invasive lobular carcinoma (ILC) masses. The system’s sensitivity dropped to 71% for invasive carcinoma masses of other types. It registered 100% sensitivity for ductal carcinoma in situ (DCIS) masses, Malich said. Roughly similar sensitivity numbers were found for microcalcifications: 91% for DCIS, 91% of IDC, 100% of ILC, and 89% of invasive carcinomas of other types.
In general, Malich’s team found that lesion size and histopathology did have an impact on CAD performance, and the overall tumor detection rate was promising. They found some drawbacks to CAD, however, such as a high false-positive rate for masses, and lower performance for less-common carcinomas.
Other presentations covered early experiences with the Second Look system. Researchers at the Institute for Diagnostic Radiology in Erlangen, Germany examined 800 mammograms of 200 patients, with radiologists of different experience levels reviewing the images.
They found that CAD improved the sensitivity of all the readers by up to 25%, regardless of experience, said the study’s presenter, Dr. Rüdiger Schulz-Wendtland. However, less-experienced readers tended to report more false-positives, he said, while more experienced readers tended to have the same false-positive rate regardless of whether they used CAD.
In addition, double reading by two radiologists showed comparable results to one radiologist working with CAD. "Despite the low specificity of the CAD system, sensitivity in mammography can be increased with experienced as well as inexperienced investigators," Schulz-Wendtland said. "However, to avoid unnecessary biopsies, a critical command of CAD is important, and with inexperienced investigators the specificity goes down. Therefore, CAD is a very fine tool in the hands of experienced investigators."
Two other studies sounded cautionary notes regarding CAD. French researchers found that the CAD system was useful for highlighting subtle abnormalities, but sensitivity depended on the types of abnormalities detected, and large lesions were often missed. The researchers said that CAD cannot yet replace a second reader, but can help the first and second readers.
Finally, an Italian group found that CAD was slightly more sensitive compared to double reading (97% versus 96%), but also increased the recall rate (7.9% versus 11.4%). CAD requires further study before it can be recommended as a replacement for double reading in routine clinical practice, the group said.
By Brian CaseyAuntMinnie.com staff writer
March 1, 2002
Related Reading
Residents benefit from CAD for mammogram reading, November 29, 2001
CAD cuts false negatives, increases sensitivity of breast imaging, November 28, 2001
CADx gets approvable letter for Second Look system, November 28, 2001
Breast CAD system scores high sensitivity, lower specificity, March 5, 2001
Copyright © 2002 AuntMinnie.com