For breast imagers, reading digital mammography exams can be a frustrating experience. Rather than being able to use a facility's central PACS network, they have to read the images on a separate, dedicated mammography workstation -- one that often isn't connected to the Internet -- making mammography interpretation more time-consuming and less efficient than it could be.
Many of these headaches can be rectified by integrating digital mammography with PACS. But the process requires much more than just plugging in a network cable, according to Dr. William Poller, director of Allegheny Cancer Center at Allegheny General Hospital in Pittsburgh, who discussed the topic at the National Consortium of Breast Centers' (NCBC) recent annual interdisciplinary breast conference in Las Vegas. AuntMinnie.com spoke to Poller and other PACS experts about strategies for integrating PACS and digital mammography.
There are a number of good reasons for integrating digital mammography with PACS, according to Poller.
"Since breast imaging is now more than just mammography -- it includes ultrasound, MR, PET, and CT, too -- you need to integrate digital mammography into the facility's general PACS to be a fully functioning breast care center," he said. "And doing so allows you to communicate better with the referring physician, especially surgeons, about all the imaging data available for the patient."
Most digital mammography vendors sell a workstation with their device. However, for a center wanting to integrate digital mammography into its PACS network, this separate workstation doesn't fit. And that's fine, according to Poller -- in fact, losing the dedicated mammography workstation has quite a few benefits:
- There's no separate service contract, in addition to the contract already in place for the facility's general PACS network.
- There's the potential for much more storage of all those data-dense mammography scans.
- Breast imagers can use the same user interface they've already learned for other modalities, rather than having to learn a new, mammography-specific one.
- There can be one streamlined workflow pattern for all modalities.
- Disaster recovery is cheaper and more efficient.
If you're still not convinced, remember the old days and consider how your current patients would respond, Poller said.
"You'd do a mammography exam on Monday, with the recall the following Monday," he said. "The ultrasound would be the following Thursday, with the biopsy the Thursday after that. With report times at about a week after the exam, it ends up being a three- to four-week process. That's just way too long nowadays."
The goal is to be able to effectively provide any image anywhere, according to Terry Macarol, program manager for system breast imaging at Advocate Health Care in Oak Brook, IL. She and her colleague at Advocate, Tuan Bui, who is Advocate's program manager for system PACS, are working to get away from dedicated mammography workstations completely.
"The dream is to be able to click on the patient's name and see all her breast images on one workstation, and not just from our facility, but from all the others she's used, as well," Macarol said.
We want to integrate. But how?
To make the dream a reality, it's necessary to consider a few key factors in the integration process, according to Poller.
"It can be expensive to integrate digital mammography and PACS," he said. "You need a plan, you need ancillary personnel, and you need the cooperation of the breast imagers and referring physicians to make it work smoothly."
As facilities prepare to integrate digital mammography with their PACS network, Poller suggests they ask: What does the breast imager need to have available at the time of interpretation? They should also consider the best physical setup for efficient reading.
Providing priors
A breast imager needs to be able to access prior studies, and he or she also needs access to a woman's correlative ultrasound; MRI breast or PET/CT studies, if applicable; and any other information, such as results from bone scans, pathology reports, or radiology reports.
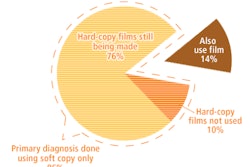
Digitizing film-screen exams was crucial to the process for Dr. Allen Nalbandian, founder of Women's Imaging Specialists (WIS) in Escondido, CA. WIS made the decision to digitize all of its priors to avoid the quasidigital mode of having to use analog and digital display equipment.
"We decided we weren't going to spend any time in purgatory, with radiologists looking at screen films, then back to the digital monitor, and vice versa," Nalbandian said. "And that was a hugely effective strategic choice in terms of our operations."
Reading areas that rock
Optimizing the physical setup for reading is crucial, Poller said. The reading area should be quiet and well ventilated, with dark walls and a user-friendly desktop. Digitize prior studies and decide what to do with outside consult studies -- whether to digitize them as well, access them via CD or DVD, or keep them as film (in which case, you'll also need a lightbox in the room).
Digitizing all priors makes for increased radiologist comfort, according to Nalbandian. "It's great. I'm still sitting there eight hours a day, but I don't have to look back and forth from the monitor to the lightbox."
Case in point
For Nalbandian, the integration of digital mammography with a general PACS network went fairly smoothly, the main reason being that WIS staff did a lot of upfront work during the planning phase.
"All that planning really paid a dividend when we went into implementation," he said.
Also key to WIS' success, according to Nalbandian:
- The facility's PACS staff created a timeline of tasks and protocols that needed to be in place before the integration happened, such as dealing with medical records and how much time would be needed to scan priors. It beefed up its staff so there would be no gaps in interpretation time.
- WIS staff worked closely with its film storage company to ensure that all the analog jackets were in order, so that no one would be scrambling for films the day the facility married digital mammography and PACS.
- WIS worked with its RIS/PACS vendor to ensure it had enough network bandwidth to accommodate the conversion (100 Mb); it also worked with its computer-aided detection (CAD) vendor to make sure the CAD data and digital data would be integrated smoothly as they were whisked off to the servers and back to the workstations.
- WIS asked its network management company to ramp up the services it had typically provided, coordinating with WIS' Internet service provider, data center company, and RIS/PACS vendor.
PACS is in the details
"In the end, you have to pay a lot of attention to the minute details," Nalbandian said. "Do not underestimate the planning process."
And paying attention to the details may mean the difference between a mediocre integration of digital mammography with PACS and a stellar one, according to Macarol: If you're going to integrate, you might as well dream big.
"How do you want the workflow to go?" she said. "What makes sense to you? You've got a blank canvas. Instead of the vendor telling you how it works, push the vendor to design the PACS to fit the mammography workflow you want."
By Kate Madden Yee
AuntMinnie.com staff writer
May 14, 2009
Related Reading
Digital mammography transition: The agony and the ecstasy, May 5, 2009
Mammography as an outpatient revenue generator? You bet, April 9, 2009
Research assesses mammography's value, April 2, 2009
Mammography procedure volume drops 16% since 2000, March 17, 2009
Radiologists overestimate breast imaging malpractice risk, February 9, 2009
Copyright © 2009 AuntMinnie.com