Computer-aided detection (CAD) is effective at finding breast cancers -- including lesions that would have otherwise been missed by experienced radiologists. Unfortunately, CAD's overall benefit is diluted by the downside of radiologists ignoring true-positive CAD marks.
"I think the novices believe the [CAD] marks and run with them, but I think we [expert readers] have already made a decision" about the lesion before the CAD is turned on, said Dr. Stamatia Destounis, a clinical associate professor of radiology at the University of Rochester School of Medicine and Dentistry, and a mammographer at Elizabeth Wende Breast Care, both in Rochester, NY.
Mammographers aren't looking their CAD gift horse in the mouth. According to Destounis, who spoke in July at the Computer Assisted Radiology and Surgery (CARS) meeting in Berlin, the 17 mammographers at the center are pretty happy overall with the high sensitivity they are achieving with their double-reading, all-soft-copy protocol combined with the use of one of two CAD systems. They just wish they had a better record of knowing when a CAD detection is true.
CAD has received a lot of scrutiny over the last several years, but has proved its worth in multiple studies and in routine clinical practice at Elizabeth Wende, Destounis said.
"As a mammographer it marks areas of concern for me, it addresses perceptual inconsistencies among interpreters," and it reduces false-negative rates, she said. "Our center has used [CAD] for all mammographies since 2000, and it has marked a lot of cancers we weren't looking at, so it was a good fit for us."
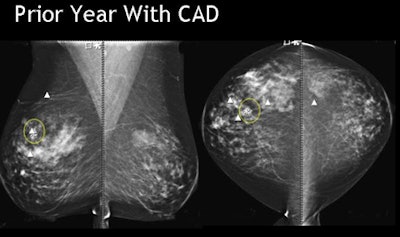 |
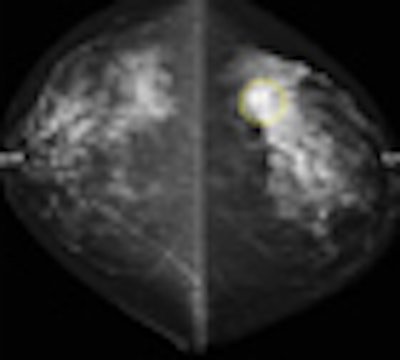
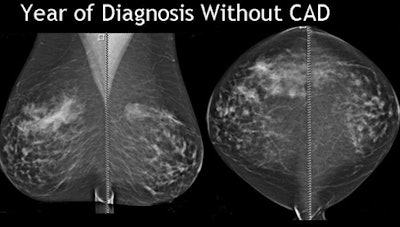
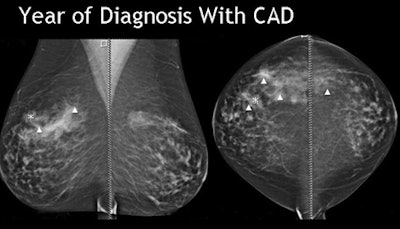
| Breast cancer detected by CAD in prior year's mammogram was ignored by the reader. All images courtesy of Dr. Stamatia Destounis. |
 |
 |
The study evaluated the effectiveness of digital mammography CAD in marking breast cancers both at diagnosis and in prior years' scans. The retrospective review examined all interval missed cancers from 2004-2008, Destounis said.
CAD, either R2 Version 8.3 (Hologic, Bedford MA) or iCAD version 7.2 (iCAD, Nashua, NH) are used by Elizabeth Wende's mammographers for all digital mammography studies, which are sent from acquisition to the CAD server, then automatically on to the PACS, Destounis said.
Two radiologists, working independently, interpret studies online and independently, Destounis said. During this process, the second reader typically knows the results of the first read.
"We started double reading back in 1993, and we looked at our own data from 1994-1996," Destounis said "We found a 9% increase in cancer detection by the second reader. We confer over our difficult cases," she added.
Retrospective review of interval and missed cancers imaged with full-field digital mammography (FFDM) between 2004 and 2008 revealed 60 cancer cases that fulfilled the study criteria. The cohort was a mixture of screening and diagnostic cases, all of which had CAD evaluation at the time of diagnosis available for review.
Digital mammography images were obtained on American College of Radiology-accredited FFDM units from Hologic, GE Healthcare of Chalfont St. Giles, U.K., and Fujifilm Medical Systems USA of Stamford, CT.
Information was collected on lesion type (mass or calcium) and location, size at mammography or surgery (if available), needle size, lymph node status, palpability, etc.
"We've pretty much moved to a vacuum needle biopsy now for most things," Destounis said. "Even for the ultrasound-guided biopsies, we've tended to move to our portable vacuum."
Ignored CAD findings
The researchers looked at CAD markings for the year of diagnosis, as well as prior years, counting the type and number of marks per view. According to the results:
- Sixty cancers were found to be visible in retrospect on prior screening or diagnostic mammograms. The average patient age was 63 years.
- BI-RADS breast density analysis revealed 22 cases (37%) with dense breasts, 21 (35%) with heterogeneously dense breasts, and 17 (28%) with scattered breast density, for total of 72% dense or heterogeneously dense cases.
- Regarding patient hormone status, 15 (25%) of the individuals were premenopausal, 45 (75%) were postmenopausal, and seven (12%) of the patients were on estrogen replacement therapy.
The 60 cases included 53 masses, five masses with calcium, one mass, and one case of calcium with architectural distortion, Destounis said.
At diagnosis CAD marked 78% (47) of the cancers, Destounis said. CAD marked 70% of the masses, 80% of masses with calcium, and missed the case of architectural distortion.
Thirteen of the 60 cancers were not detected by CAD in any view, including 11 masses, one mass with calcium, and one case of calcium with architectural distortion. There were 11 biopsy-proven invasive ductal carcinomas, one biopsy-proven atypically papillary neoplasm or DCIS, and one biopsy-proven metastatic malignant melanoma.
"CAD marked the area of cancer 47% of time (n = 24) on the prior most recent mammo, and in fact there was one case where the cancer was marked on two prior years," Destounis said. But in all cases of prior findings, either "we didn't pick it up or we didn't mark it," she said.
In 15 cases nothing was marked by the CAD in prior years, and 13 cases (27%) did not have the prior digital mammo file with CAD available for review, Destounis said.
Overall, CAD marked the cancer 78% of the time, and cancer in prior year(s) 40% of the time, she said. So the study showed that even when CAD marked the lesion of interest, radiologists continue to disregard the CAD marks frequently, she said. Why is this happening?
"The area may be a lower threshold of concern for the radiologist reading or for both of us reading at the same time," Destounis said. "Or we're distracted by something else. Frequently I'm working up the cyst on the other side, or the calcium that turns out to be benign, or a core biopsy. So I guess satisfaction of search is a factor," she said.
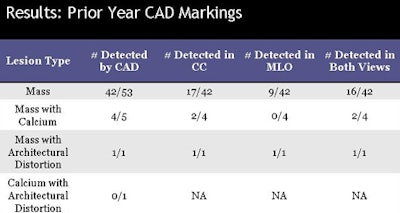 |
| Chart shows that nearly half of all breast cancers eventually diagnosed were initially detected by CAD but ignored at the prior year's digital mammography. |
In fairness to the mammographers, more than three-quarters of the cases missed by readers were unusual, with "unexpected findings," Destounis said, adding that it would be easier to believe CAD if it were accurate more than 75% of the time.
But the fact remains that many of the cancers were seen on CAD in prior years, and rejected as false positives by the radiologist. As a result, anything that helps readers believe in the accuracy of CAD marks would be helpful, she said.
But many experienced readers make their decisions in the first diagnosis -- before CAD -- and by the time they look at the CAD results, it's very difficult, especially for more experienced readers, to change their mind.
"For calcium if I've really blown by [a case] I will go back and spend a lot of time looking at it, but for masses, the difficulty is that it may be visible in only one view or even in a three-year prior [study]," she said. "I try to look at priors because if it's a developing density you're not going to see it."
By Eric Barnes
AuntMinnie.com staff writer
October 23, 2009
Related Reading
Fuzzy 3D ultrasound CAD sharpens breast cancer sensitivity, September 3, 2009
Breast ultrasound CAD helps doctors find smaller lesions, October 10, 2008
CARS report: CAD prompts range of behaviors in readers, June 26, 2008
Breast CAD improves classification accuracy, cuts ultrasound biopsies, February 29, 2008
Breast MRI CAD doesn't improve accuracy due to poor DCIS detection, February 18, 2008
Copyright © 2009 AuntMinnie.com