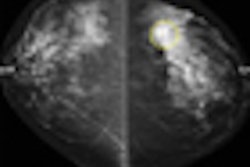
Biennial mammography screening achieves most of the benefit of annual screening with less harm, according to a new study conducted by researchers from the breast cancer working group of the Cancer Intervention and Surveillance Modeling Network (CISNET).
Published November 17 in the Annals of Internal Medicine, along with the U.S. Preventive Services Task Force's (USPSTF) controversial new recommendation that women not start screening until after age 50, the study used six models of breast cancer incidence and mortality in the U.S.
"These models are ideally suited for estimating the effect of screening under a variety of policies," wrote lead author Dr. James Mandelblatt of Georgetown University Medical Center in Washington, DC. "Modeling has the advantage of being able to hold selected conditions (for example, screening intervals or test sensitivity) constant, which facilitates comparison of strategies."
Mandelblatt and colleagues found that screening biennially maintained an average of 81% of the benefit of annual screening with almost half the number of false-positive results. (The range of benefit across all six models was 67% to 99%.) Screening women ages 50 to 69 every other year produced a median 16.5% reduction in breast cancer deaths compared to no screening at all. The study lists false positives, unnecessary biopsies, and overdiagnosis as "harms" of annual screening.
Starting biennial screening for women ages 40 or older didn't add much benefit, the team wrote.
"Initiating biennial screening at age 40 years (versus 50 years) reduced mortality by an additional 3%, consumed more resources, and yielded more false-positive results," the researchers wrote.
The CISNET study bolsters USPSTF's recommendation that screening should start at 50 instead of 40 and be performed every other year, a recommendation that has sparked huge controversy, with advocacy groups such as the American College of Radiology (ACR) of Reston, VA, arguing that the new advisory will place women at risk.
Mandelblatt's team acknowledged that the study results are contrary to "current practices in the United States" and that "whether it will be practical or acceptable to change the existing U.S. practice of annual screening cannot be addressed by our models."
"Our result that biennial screening is more efficient than annual screening is consistent with previous modeling research and screening trials, most of which used two-year intervals," Mandelblatt added. "Our results are also consistent with current knowledge of disease biology. Slow-growing tumors are much more common than fast-growing tumors, and the ratio of slow- to fast-growing tumors increases with age, so that little survival benefit is lost between screening every year versus every other year."
Related Reading
USPSTF ups mammography screening age to 50, November 16, 2009
JAMA editorial raises questions about breast, prostate screening, October 22, 2009
Shock and awe over JAMA editorial, October 22, 2009
'Spontaneous regression' debate erupts anew at ASCO symposium, October 12, 2009
Most breast cancer deaths seen in nonscreened women, October 7, 2009
Copyright © 2009 AuntMinnie.com