Conebeam breast CT can image the entire breast from chest wall to nipple with sufficient resolution and at a radiation dose within the range of conventional mammography, according to a new study published in the August issue of the American Journal of Roentgenology.
Lead author Avice O'Connell, MD, from the University of Rochester Medical Center in Rochester, NY, and colleagues conducted a pilot study between July 2006 and August 2008 to evaluate radiation dose, breast coverage, and image quality of conebeam breast CT as compared to conventional mammography (AJR, August 2010, Vol. 195:2, pp. 496-509).
Despite the fact that mammography is the gold standard for early detection of breast cancer, it does have limitations, one of which is that it's a 2D technology imaging a 3D structure, which can make seeing some cancers difficult. As a 3D technology, conebeam breast CT has the potential to overcome this particular limitation. But concerns about its radiation dose and whether it can provide adequate breast coverage compared to mammography remain.
The current study included 23 women who were 40 years or older, with a BI-RADS 1 or 2 category on a conventional mammogram within the previous six months. The team imaged the women using a flat-panel detector-based conebeam CT unit (Varian Medical Systems, Palo Alto, CA) and viewed the images with 3D software. The researchers then compared the conebeam CT images to the women's conventional mammograms.
Average glandular radiation dose for conventional mammography was 2.2 mGy to 15 mGy; for conebeam CT breast imaging, it was 4 mGy to 12.8 mGy. The difference between mean glandular doses of conventional mammography and conebeam breast CT in dense breasts was not statistically significant, according to O'Connell.
"The glandular dose from conebeam breast CT was within the range of the glandular dose from conventional mammography," O'Connell and colleagues wrote. "This dose range ... is acceptable because the intended use of conebeam breast CT is diagnostic imaging."
Conebeam CT had better breast tissue coverage for the lateral, medial, and posterior imaging aspects (92.5% versus 12.5%, 90% versus 35%, and 90% versus 52.5%, respectively), while mammography performed better than conebeam CT in the axilla and axillary tail aspects (72.5% versus 7.5%).
As for image quality, conebeam CT detected 89.6% of the findings mammography had located, or 60 out of 67 (with a size range of 1 mm to 15 mm).
"Mammography was better than conebeam breast CT at depicting the details of calcifications because calcifications, especially those 1 mm in diameter and larger, on conebeam breast CT scans are subject to beam-hardening artifact," they wrote.
There was size agreement between conebeam CT and mammography in 60% of the findings that were detectable by both systems and for which size information was available. Agreement between mammography and conebeam breast CT for the location of findings was 70%. As for image conspicuity, conebeam breast CT performed better than mammography, which the authors attributed to the breast tissue not being compressed.
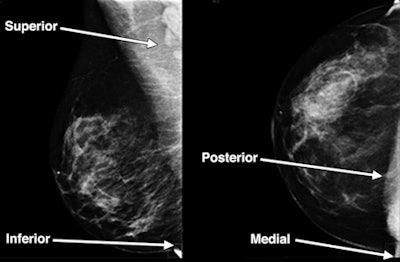 |
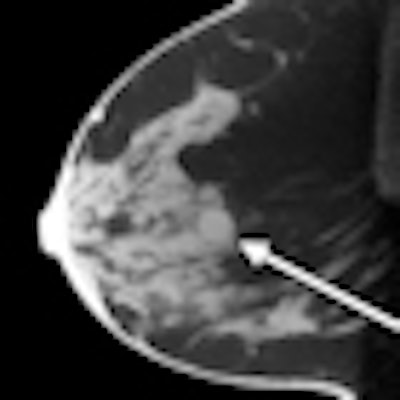
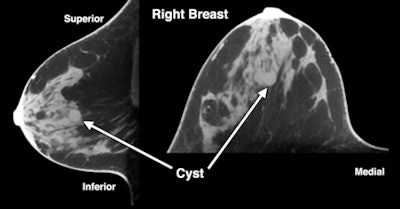
| Images are of a 47-year-old woman with a sonographically proven 0.8-cm benign cyst. Above: Mediolateral oblique (left) and craniocaudal (right) digital mammograms do not clearly show a benign cyst. Below: Sagittal and transverse conebeam breast CT images corresponding to the images above show a benign cyst differentiated from surrounding breast parenchyma owing to lack of structure overlap. Images courtesy of the American Roentgen Ray Society. |
 |
Reader agreement between the two modalities was 77.2% for type of findings, 84.8% for size of findings, and 78.3% for location of findings, the team noted.
Finally, the study showed an added benefit to conebeam breast CT: Women experienced less discomfort with the technology than with conventional mammography. Forty-four percent of the women in the study reported that conebeam breast CT was more comfortable than mammography, and 43% reported that conebeam breast CT was equivalent in comfort to mammography, according to the researchers.
"One of the great advantages of conebeam breast CT in terms of patient tolerance is the lack of breast compression with retention of sufficient image quality for potential clinical applications," they wrote. "Compression has been the most common complaint about mammography because of patient discomfort."
O'Connell did not report any disclosures with the study, but several study co-authors reported employment or financial ties to conebeam CT developer Koning of West Henrietta, NY.
By Kate Madden Yee
AuntMinnie.com staff writer
July 27, 2010
Related Reading
CARS report: Novel conebeam CT cuts breast dose, improves accuracy, June 29, 2009
ECR delivers new findings on digital breast tomosynthesis, March 7, 2009
Italian study backs tomosynthesis over DR for lung pathology, February 18, 2009
New breast imaging applications show diagnostic promise, January 20, 2009
Pilot study: DBT's role needs further research, April 18, 2008
Copyright © 2010 AuntMinnie.com