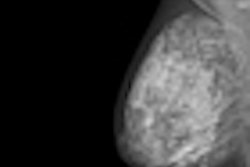
A new study from researchers at Brigham and Women's Hospital indicates that the rarity of breast cancer may contribute to the relatively high miss rate found in screening mammography, in which radiologists are estimated to miss 20% to 30% of cancers.
Jeremy Wolfe, PhD, of Brigham and Women's shared findings at the recent RSNA 2011 conference in Chicago from a study he conducted with colleagues that examined the association between low disease prevalence and high miss error rates in the clinical setting.
"Miss error rates in screening mammography are estimated to be 20% to 30%," Wolfe told session attendees. "But the prevalence of breast cancer in a screening population is very low, about 0.3%. The surprise is that we find greatly elevated miss errors at low prevalence as compared to lower miss errors when the target appears at high prevalence, that is, at least 50% of the time."
Wolfe's group conducted the study under two research arms: low prevalence and high prevalence. In the low-prevalence arm, 100 cases (50 positive, 50 negative) were inserted into normal screening workflow over nine months, so as to have minimal impact on normal practice. Including the inserted cases, prevalence of disease was about 1%. In the high-prevalence arm, six radiologists read the same 100 cases in a single three-hour session.
At high prevalence, the breast cancer miss error rate was 12%. The miss rate rose to 30% at low prevalence for the same set of 100 cases, Wolfe said. Most of the cancers that were missed at low prevalence were found when seen in the high-prevalence arm.
"This prevalence effect is adaptive in most real-world settings, where an observer should be reluctant to assert that she has found a very rare target such as UFOs, Elvis, or ivory-billed woodpeckers," Wolfe said. "However, in mammography, a task invented by modern civilization, this strongly ingrained behavior may be counterproductive."
Why should radiologists care about this phenomenon? Because it happens in regular practices, Wolfe said. And it's something considered "cognitively impenetrable" -- that is, one can't talk oneself out of it.
"What is interesting [about these findings] is that it's radiologists reading cases under regular circumstances," Wolfe said. "The source of the errors is the interaction of the radiologist's nervous system with the task, not poor imaging or the skills of specific radiologists. And it's not easy, even for an observer radiologist, to tell himself, 'I'm working in a low-disease-prevalence setting, but I'm going to act like it's a high-prevalence setting."
What can practices do to counteract the low-prevalence effect? One idea is to give radiologists a kind of "booster shot" --- a chance to read a series of studies quickly that have cancers present 50% of the time and get immediate feedback on whether they were right. For example, radiologists could start the day off with three or four minutes of a rapid-fire "find the cancer" quiz, and in that way prime their brains to see breast cancers they might have missed, according to Wolfe. He and his colleagues hope to put such an experiment in place in the coming year.
"The problem is when you're looking for something rare and don't get any feedback when you do find it, your brain adopts a conservative response -- 'That can't be cancer,' " Wolfe told AuntMinnie.com. "At least in the lab, we've found that if you give people a burst of practice [finding something rare] a high prevalence for a few minutes and give them feedback, it kind of resets the brain."