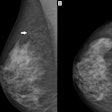
It's time to move on in the debate over screening mammography's effectiveness, according to Australian researchers, who found that mammography reduces breast cancer mortality by 49%. They reported their results in a paper this month in Cancer Epidemiology, Biomarkers & Prevention.
Researchers from the University of Melbourne in Victoria conducted a case-control study of breast cancer deaths in Western Australia to assess the effect of participation in BreastScreen Australia, a population-based screening program that has provided free biennial mammographic screening since the mid-1990s (Cancer Epidemiol Biomarkers Prev, September 2012, Vol. 21:9, pp. 1479-1488).
Women ages 50 to 69 are directly invited to participate in BreastScreen Australia, while women ages 40 to 49 are eligible but not directly invited. Since 1996, biennial participation in the target age group of 50 to 69 years has ranged from 52% to 57%, wrote lead author Dr. Carolyn Nickson and colleagues from the Melbourne School of Population Health.
"It is important that Australian women have accurate information about the pros and cons of participating in BreastScreen," Nickson said in a statement. "The findings of this study may help women decide whether to participate."
To evaluate the potential effect of biases discussed in the literature on case-control studies of screening, the group conducted several sensitivity analyses (including selection, information, and confounding data biases). Nickson and colleagues also performed a meta-analysis of case-control studies evaluating mammographic screening.
The study focused on women ages 50 to 69 years, who are in the target age range for screening. It included 427 cases where women had died from breast cancer and 3,650 control women who were still alive when the other women died. The researchers compared screening attendance between the two groups and found screening rates were much lower among women who had died from breast cancer.
The odds ratio for participation in the Western Australian BreastScreen program in relation to death from breast cancer was 0.48 (p < 0.001). Nickson's group did not discover biases that went against this finding: Sensitivity analyses generated odds ratios from 0.45 to 0.52 (for an average of 0.49). The team's meta-analysis found an even higher odds ratio of 0.51.
The study findings reaffirm the importance and efficacy of mammography, according to Nickson and colleagues.
"Sound research methods have been used in this study," Nickson said. "I believe it is time to move on from the debate about whether screening reduces mortality and to instead direct research resources to help improve the program for women who choose to use it."