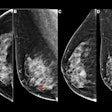
Breast screening programs do extend lives and overall the benefits outweigh the harms, but overdiagnosis remains a serious cause for concern and requires more attention, an independent U.K. panel has found.
Routine breast screening leads to a 20% relative risk reduction compared with no screening. This means that for every 235 women invited for screening, one breast cancer death will be prevented, representing 43 breast cancer deaths prevented per 10,000 women age 50 years invited to screening for the next 20 years, according to a team led by Dr. Sir Michael Marmot, PhD, a professor of epidemiology and public health, the director of the Institute of Health Equity at University College London, and a leading public health academic.
 More research is needed to accurately assess the magnitude of overdiagnosis, according to Dr. Sir Michael Marmot, chair of the Independent Breast Screening Review.
More research is needed to accurately assess the magnitude of overdiagnosis, according to Dr. Sir Michael Marmot, chair of the Independent Breast Screening Review.
But the researchers' report, published online today by Lancet, is unlikely to draw a line under the ongoing debate. On the downside, they estimate that 19% of breast cancers diagnosed in women invited for screening would not have caused any problem if left undiagnosed and untreated -- a rate of 129 per 10,000 women. Given the scarcity of reliable data in this area, Marmot's group thinks more research is needed to accurately assess the magnitude of overdiagnosis.
"Dissemination of these findings is now imperative in the media, the NHS [National Health Service] screening program, and between doctors and their patients," noted an accompanying Lancet editorial. "Women need to have full and complete access to this latest evidence in order to make an informed choice about breast cancer screening."
The panel was set up by Dr. Sir Mike Richards, the U.K.'s national clinical director for cancer, and Dr. Harpal Kumar, CEO of Cancer Research UK. The aim was to reach conclusions about the benefits and harms of breast screening on the basis of a review of published work and oral and written evidence. The panel relied mainly on findings from randomized trials of breast cancer screening that compared women invited to screening with controls not invited, but it also reviewed evidence from observational studies. In the U.K., women ages 50 to 70 are invited to screening every three years.
Three types of uncertainty surround the panel's estimate of the relative risk reduction of 20%. The first is statistical: The 95% confidence interval (CI) around the relative risk of 0.80 was 0.73 to 0.89. The second is bias: During the decades since these trials were reported, there has been much discussion of their internal validity. The third is the relevance of these old trials to current screening programs. The panel concluded that 20% was still a reasonable estimate of the relative risk reduction. The more reliable and recent observational studies generally produced larger estimates of benefit, but these studies might be biased, it noted.
There is no single optimum way to estimate overdiagnosis, but the authors think the two most useful estimates are, from the population perspective, the proportion of all cancers ever diagnosed in women invited to screening that are overdiagnosed, and, from the perspective of a woman invited to screening, the probability that a cancer diagnosed during the screening period represents overdiagnosis.
The best estimates of overdiagnosis are from three trials in which women in the control group were not invited to be screened at the end of the active trial period, they said. Results from observational studies support the occurrence of overdiagnosis, but estimates of its magnitude are unreliable. Of the roughly 307,000 U.K. women ages 50 to 52 who are invited to begin screening every year, just more than 1% would have an overdiagnosed cancer in the next 20 years.
"Many women feel that accepting the offer of breast screening is worthwhile, which agrees with the results of previous similar studies. Information should be made available in a transparent and objective way to women invited to screening so that they can make informed decisions," the authors stated.
The panel recommends that the U.K. breast screening programs should continue. "For each woman, the choice is clear. On the positive side, screening confers a reduction in the risk of mortality from breast cancer because of early detection and treatment. On the negative side is the knowledge that she has perhaps a 1% chance of having a cancer diagnosed and treated that would never have caused problems if she had not been screened."
The panel supports the ongoing meta-analysis of centrally collated individual patient data from all the randomized trials. It also backs the use of randomized trials to investigate the balance of benefit to harm of breast cancer screening to women younger than 50 and those older than 70. But it noted that further research is needed to improve the precision of screening to better distinguish between breast cancers that will or will not cause harm during a woman's lifetime. Randomized trials that elucidate the appropriate treatment of screen-detected ductal carcinoma in situ of different grades also are encouraged, and there is a need for better understanding of the natural history of ductal carcinoma in situ, the authors concluded.
To read more about the report, click here.