Digital breast tomosynthesis (DBT) is more accurate than mammography for working up suspicious findings on screening exams, which could translate into fewer recalls and unnecessary biopsies, researchers from Pittsburgh report in the January issue of Radiology.
Lead author Dr. Margarita Zuley and colleagues from the University of Pittsburgh compared the diagnostic performance of breast tomosynthesis to supplemental mammography in the classification of masses, distortions, and asymmetries. The group found that when radiologists used tomosynthesis, they rated fewer benign masses as probably or definitely malignant -- BI-RADS categories 3, 4, or 5 -- without a loss of sensitivity.
 Dr. Margarita Zuley from the University of Pittsburgh.
Dr. Margarita Zuley from the University of Pittsburgh.
"In clinical practice, the results of this study suggest that use of tomosynthesis is likely to translate into fewer recalled screening examinations, fewer short-interval follow-up studies, and fewer biopsies in patients with benign lesions," Zuley and colleagues wrote (Radiology, January 2013, Vol. 266:1, pp. 89-95).
Radiologists already use supplemental diagnostic mammography to evaluate possible abnormalities. The views are acquired in addition to the standard mediolateral oblique (MLO) and craniocaudal (CC) views and include angled, rolled, or spot compression views (with or without magnification).
Such views, however, do not necessarily contribute helpful clinical information, according to Zuley's group: The average positive predictive value of an abnormal interpretation in the diagnostic setting, even with these supplemental views, is less than 36%. The authors felt that tomosynthesis might enable better characterization of suspicious findings.
To evaluate this hypothesis, eight breast imaging radiologists retrospectively reviewed 217 lesions in 182 patients who underwent diagnostic mammography and tomosynthesis. Of the lesions in the cohort, 33% (72) were cancers and 67% (145) were benign.
Of the 217 lesions, 8% were initially detected at clinical examination, 80% at mammography, 11% at ultrasound, and 1% at MRI, according to Zuley's group. Most were masses (84%, or 182 of 217), while 11% (25) were asymmetries and 5% (10) were distortions.
The study's radiologists interpreted each lesion once with tomosynthesis and once with supplemental mammography. Using receiver operator characteristics (ROC) analysis, the researchers found that radiologists using DBT were more accurate in assessing the malignancy of a suspicious lesion. Tomosynthesis had an area under the ROC curve of 0.87, compared with 0.83 for supplemental mammography.
In addition, with tomosynthesis, the false-positive rate decreased from 85% to 74% for cases rated BI-RADS category 3 or higher and from 57% to 48% for BI-RADS category 4 or 5 cases -- without a meaningful change in sensitivity. More cancers were also classified as BI-RADS category 5 with DBT (39% versus 33% for additional views) without a decrease in specificity.
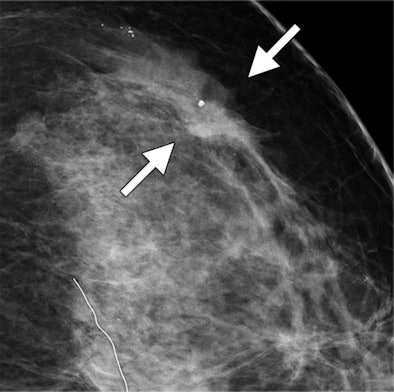 |
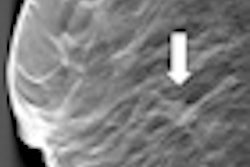
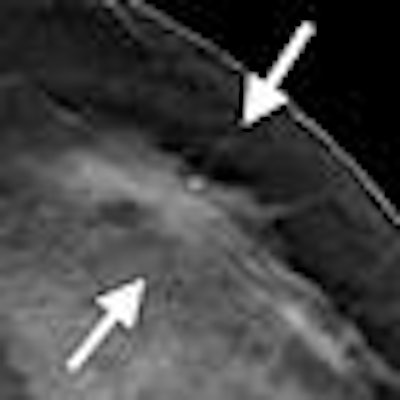
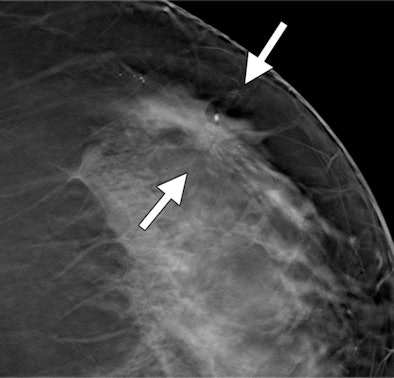
| Images show possible mass in a 54-year-old woman. Craniocaudal spot compression (above) and tomosynthesis (below) show biopsy-proved invasive ductal carcinoma (arrows). The spiculated mass margins are better shown with DBT than in the spot compression image. All images courtesy of RSNA. |
 |
Anything that streamlines the diagnostic process is good news for both radiologists and patients, Zuley told AuntMinnie.com.
"We want to be able to take care of patients with less radiation exposure, more accuracy, and more efficient workflow," she said. "If you look at the bigger controversy around mammography, tomosynthesis addresses a number of the [cited harms of overuse]: It reduces the recall rate, it has higher sensitivity and accuracy, and the time it takes to work up a patient is less, so it may reduce patient anxiety."