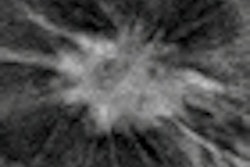
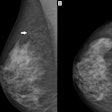
Digital breast tomosynthesis (DBT) could replace conventional diagnostic mammography for further workup of noncalcified lesions found on screening mammography, according to a study published in the February issue of the American Journal of Roentgenology.
Researchers from the Mayo Clinic in Rochester, MN, found no significant difference between DBT and diagnostic mammography in terms of sensitivity, specificity, or accuracy. Using DBT instead of mammography could not only reduce the time required, it could also perhaps reduce a woman's radiation exposure from additional mammographic views acquired during workup.
"If shown to be adequate, DBT might more quickly be incorporated into diagnostic breast imaging practices," hypothesized lead author Dr. Kathleen Brandt and colleagues.
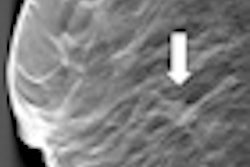
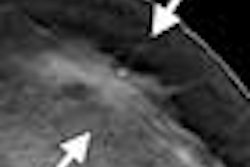
Supplemental mammographic images, such as spot compression views, are often acquired when abnormal findings are detected on screening mammography, and they have been shown to improve mammography's specificity, Brandt's team wrote. Clinical studies have established that DBT is at least equivalent to mammography for this purpose (although mammography does tend to do better with calcified lesions), but no study has included a full range of data that would be available in a clinical setting, such as comparison mammograms and breast ultrasound results (AJR, February 2013, Volume 200:2, pp. 291-298).
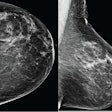
To investigate this issue, the researchers included 146 women with 158 abnormalities in the patient cohort. The women underwent both diagnostic mammography and two-view DBT; the diagnostic mammography evaluation may have included digital spot compression views with or without magnification, rolled views, lateral views, exaggerated views, and ultrasound, depending on the breast radiologist assigned to the clinic at the time, the authors wrote.
Three study radiologists viewed the abnormal screening mammograms, comparison mammograms, and DBT images and recorded a DBT BI-RADS category and confidence score for each finding. The three readers did not see the diagnostic mammograms.
The readers used the following three-point scale to rate their confidence:
- Additional conventional mammographic views and ultrasound needed.
- Ultrasound needed for further evaluation; ultrasound findings (positive or negative) would be accepted as final result.
- No additional imaging needed for final BI-RADS assessment; if ultrasound is performed, the only reason would be to determine whether ultrasound could guide biopsy.
For each case, Brandt and colleagues determined a final DBT BI-RADS category -- including ultrasound results in some cases -- and compared it to diagnostic mammography findings using kappa statistics (a kappa value of 1 indicates perfect agreement, while 0 indicates chance agreement). The group then calculated the sensitivity and specificity of both DBT and diagnostic mammography.
For readers 1 and 2, agreement between DBT and diagnostic mammography BI-RADS categories was "excellent" (kappa = 0.91 and 0.84); agreement was "good" for the third reader (kappa = 0.68). The team found that DBT's sensitivity, specificity, and accuracy (with or without ultrasound) were high among all three readers and compared well to the sensitivity, specificity, and accuracy of the diagnostic mammography exams.
DBT vs. mammo (with or without US)
|
Results of confidence scores showed that readers 1 and 2 considered two-view DBT to be adequate mammographic evaluation for 99% of the findings; reader 3 considered it adequate for 93%. Readers 1, 2, and 3 would have ordered breast ultrasound for further evaluation in 44%, 28%, and 48% of cases, respectively. They would have ordered breast ultrasound only to determine whether that technology could be used to guide biopsy in an additional 5%, 4%, and 7% of the cases, Brandt's team found.
DBT could reduce the number of additional mammographic views taken during diagnostic workup, the authors concluded: The conventional diagnostic mammography workup included a median of three additional views, and positioning for these views, particularly spot compression, can be challenging.
"Positioning for DBT is much simpler, being identical to positioning for routine mammography, and the problem with tissue superimposition is greatly reduced," they wrote. "Thus, DBT has potential to reduce the number of additional mammographic views obtained during a diagnostic workup and improve technologist efficiency."