VIENNA - Mammography is an imperfect modality -- more so than many others -- so it makes sense that radiologists are on the lookout for something better, or at least something to supplement the technique. This afternoon's refresher course covers functional imaging of the breast and goes into detail about ultrasound elastography, contrast-enhanced mammography, and MRI diffusion, perfusion, and spectroscopy, which may supplement mammography or replace it altogether.
Ultrasound elastography has been around since the 1980s and emerged as a complementary technique to estimate local tissue stiffness. There are two main types: strain imaging (externally applied compression using the probe and creating a local tissue deformation) and shear-wave imaging (no external compression, shear-wave emission, and propagation through the tissue is responsible for local tissue displacement). Its utility has already been established for use in liver cirrhosis, as well as breast, prostate, and thyroid lesions.
"Breast elastography is indeed helpful in providing further information about breast lesion stiffness, the point being that cancers are stiffer than benign lesions and lesions having a similar B-mode aspect could be further differentiated as benign or malignant according to their stiffness (i.e., their elastic value)," noted Dr. Alexandra Athanasiou, from the radiology department at the Institut Curie in Paris.
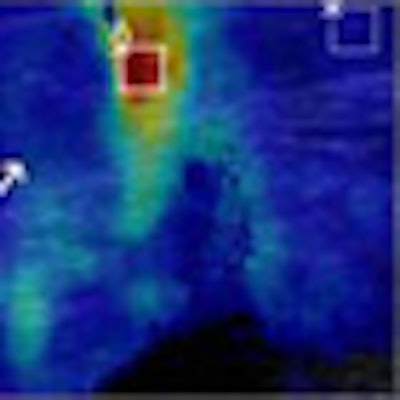
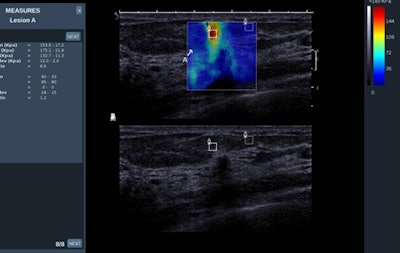 This clinical case is of a small infiltrating ductal carcinoma coded as red, i.e. elevated elasticity value. The resolution of the technique is 1 mm. Image courtesy of Dr. Alexandra Athanasiou.
This clinical case is of a small infiltrating ductal carcinoma coded as red, i.e. elevated elasticity value. The resolution of the technique is 1 mm. Image courtesy of Dr. Alexandra Athanasiou.Numerous studies have already been published to validate breast elastography, and further research is ongoing in order to define elastography criteria, she added. It's important to note breast ultrasound elastography will be part of the new edition of the BI-RADS lexicon for ultrasound.
Strain elastography provides qualitative or semiquantitative information, whereas shear-wave imaging provides quantitative values of elasticity and is more operator-independent, she explained.
"Breast imagers will have to be familiar with ultrasound elastography -- new BI-RADS criteria will enhance this necessity," Athanasiou stated. "A good understanding of basic physics is important in order to correctly perform elastography -- whether strain or shear wave -- and correctly interpret findings."
ECR delegates will get exactly that during her presentation. She aims to cover basic physics, along with the clinical applications and pitfalls of breast ultrasound elastography. Attendees will also receive information on how to perform and interpret findings.
"A review of literature will also be provided in order to give clear messages on what to expect from breast ultrasound elastography in the actual technical and clinical setting," she added.
 Dr. Corinne Balleyguier, from Institut Gustave Roussy (IGR) in Villejuif, France.
Dr. Corinne Balleyguier, from Institut Gustave Roussy (IGR) in Villejuif, France.
In the same session, Athanasiou's colleague, Dr. Corinne Balleyguier, from Institut Gustave Roussy (IGR) in Villejuif, France, will present on contrast-enhanced spectral mammography (CESM), which was highlighted at the 2012 RSNA congress, when German researchers suggested symptomatic women could be spared from unnecessary radiation by skipping regular mammography and going straight to contrast-enhanced spectral mammography.
The technique combines digital mammography and injection of an iodinated contrast agent. Mammography images are acquired at high and low energy levels.
"There is some mandatory hardware adaptation, for instance adding a copper filter and dedicated software is required. However, interpretation of images is based on morphological criteria," said Balleyguier, who will expand on the topic and discuss the underlying physical principles, protocols, and the potential impact on everyday clinical practice."
The radiation dose is 1.2 times that of a normal digital mammogram. The indications for CESM are similar to that of MRI.
"CESM significantly improves characterization of breast lesions as compared with mammography," she said. "For breast cancer staging, as compared with MRI, CESM carries a slightly lower sensitivity, but conversely a better specificity, cutting down the number of false positives."
There are some false negatives but, nonetheless, CESM might become a very practical, cost-saving alternative to breast MRI in specific clinical situations, she added.
Delegates can also expect to learn about MRI diffusion, perfusion, and spectroscopy from Dr. Pascal Baltzer at the University of Jena in Germany.
"Dynamic contrast-enhanced MR mammography is the most sensitive method for detection of breast cancer," he said. "Diagnostic results using this technique may vary due to reader experience as image interpretation is to some degree a subjective task."
Other MRI techniques have been investigated, but while pharmacokinetic modeling of high temporal resolution dynamic contrast-enhanced imaging promises further quantitative insights into the pathological characteristics of neoplastic vasculature, diffusion-weighted imaging (DWI) and MR spectroscopy (MRS) are based on entirely different concepts, he said.
"While MRS is a molecular imaging technique able to quantify biochemical tissue properties, DWI is influenced by microstructural tissue changes," remarked Baltzer, who promises to outline the concepts of perfusion, DWI, and MRS, to provide knowledge to implement these techniques into clinical practice, and to critically discuss the possible diagnostic benefit of doing so.
Originally published in ECR Today on 7 March 2013.
Copyright © 2013 European Society of Radiology