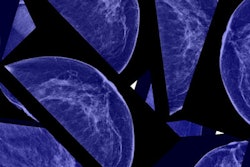
Mammography skeptic Dr. Gilbert Welch has published a new article in JAMA Internal Medicine intended to add some clarity to the debate over mammography screening by quantifying its benefits and harms. But mammography proponents are questioning a number of Welch's conclusions.
Welch was a co-author on a controversial article published in November 2012 in the New England Journal of Medicine that questioned the effectiveness of mammography relative to the risk of overdiagnosis.
The problem is quantifying that risk, as few studies to date offer information on the frequency of overdiagnosis and its relationship to cancer detection, wrote Welch and co-author Honor Passow, PhD, both of the Dartmouth Institute for Health Policy and Clinical Practice. They aim to correct that deficiency in the current article (JAMA Intern Med, December 30, 2013).
"Simply knowing that there are benefits and harms to screening is not sufficient to make the decision; information about their relative magnitude is essential," they wrote.
Quantifying outcomes
Welch and Passow decided to quantify three of the main outcomes related to screening mammography for women ages 40 to 60: reduction in breast cancer death; false-positive results (including breast biopsies); and overdiagnosis, or the number of patients treated for cancer that would never have represented a health risk during their lifetime. The researchers calculated the outcomes in a hypothetical population of 1,000 women in the U.S. who were screened for 10 years.
For each of the three main outcomes, the authors created a range that represented both the most optimistic and most pessimistic scenarios, based on studies in the literature. To calculate the high end of mammography's impact on breast cancer death, for example, they used data from the Swedish Two-County Trial, generally viewed as the most optimistic, and calculated a 36% mortality reduction; for the bottom of the range, they based their estimate on the Canadian mammography trials and assumed a 5% reduction.
Welch and Passow then calculated mortality reductions over 15 years after the start of breast screening for women age 50 who underwent annual screening for 10 years. At the most optimistic end of the scale, mammography produced a mortality reduction of 3.2 lives per 1,000 women; at the other end of the scale, the mortality benefit was only 0.3 lives per 1,000 women.
With respect to false positives (which the authors define as screening exams that require repeat or recall mammography studies), the authors used data from a 2011 study by Hubbard et al in Annals of Internal Medicine, which found that women receive one false-positive mammogram each decade. Based on the data, Welch and Passow estimated that 490 to 670 recalls and 70 to 100 false-positive biopsies would take place per 1,000 women over a 10-year course of screening mammograms.
Finally, in analyzing overdiagnosis, Welch and Passow used long-term follow-up of the Malmö randomized trial of screening mammography, a 15-year trial that the authors said represents "the highest-quality evidence that overdiagnosis is a consequence of screening mammography." They also estimated that one-third of all detected cancers represent overdiagnosis, meaning there would be 14 cases of overdiagnosis in their hypothetical population of 50-year-old women screened for 10 years. Reducing the screening frequency to every two years would reduce false positives by half, and would be expected to reduce the rate of overdiagnosis as well.
Welch and Passow then produced three charts that quantified the risks and harms of mammography for women ages 40, 50, and 60 at the start of a 10-year screening regimen.
| Benefits vs. harms of screening mammography per 1,000 women | |||
| Age | Mortality reduction | No. of women with at least 1 false alarm | No. of women overdiagnosed |
| 40 | 0.1-1.6 lives saved | 510-690 | ?-11 |
| 50 | 0.3-3.2 lives saved | 490-670 | 3-14 |
| 60 | 0.5-4.9 lives saved | 390-540 | 6-20 |
In a related editorial in the New York Times on December 29, Welch acknowledged that while the above data could help some women decide whether to undergo screening, the information is still not very precise. He also pointed out that much of the data in the current study are based on trials performed 25 to 50 years ago.
He proposed a new round of two randomized clinical trials: In one, women would be examined with either the current approach or a "high-threshold approach," in which radiologists would ignore small abnormalities not likely to be cancer. The second trial would pair women using the high-threshold approach with those who were not screened at all.
It would be expensive to conduct the trials; however, the costs pale in comparison to what is currently being spent on breast screening.
"Putting the two trials together, we could finally learn what level of screening minimizes false alarms and overdiagnosis while saving the most lives," Welch wrote in the New York Times.
At least one mammography proponent -- Dr. László Tabár of Falun Central Hospital in Sweden -- disagrees with the conclusions of the new article. In an email to AuntMinnie.com, Tabár objected to the methodology of the study, as well as a suggestion by Welch and Passow that the more-effective therapies available today make it less imperative to discover cancer early; in the New York Times piece, Welch characterizes women developing breast lumps as a form of "early diagnosis."
"Welch extols the magical effect of modern therapeutic regimens, but neglects to mention that women with lymph node metastases have a significantly worse outcome than women with node-negative tumors; this nullifies his main argument," Tabár said. "On the other hand, he scorns the eight population-based randomized, controlled trials that proved the significant mortality benefit of early detection and treatment in the early phase of breast cancer."
The new study has also drawn fire from Dr. Daniel Kopans of Massachusetts General Hospital. Kopans charges that Welch in his statements in the New York Times editorial misunderstands many of the main issues involved in analyzing breast screening, such as his statement of performing a randomized clinical trial in which women could choose which arm of the study to participate in.
"What he describes are simply not 'randomized trials,' " Kopans wrote in an email to AuntMinnie.com. "If you chose to be in one group or the other, this is not 'random' and it introduces the well-known problem of 'selection bias.' No scientist would accept this type of study design because the results would be unreliable."
He also disputes Welch's statement of the benefits of mammography after a lump has been detected.
"Welch has repeated this misinformation over and over again," Kopans wrote. "In fact, there is no lifesaving benefit from having a mammogram once a lump has developed. The benefit comes from finding the cancer before it is large enough to be a lump. Every doctor who cares for women with breast cancer knows this. Why is finding a lump a 'form of early diagnosis that we all agree on,' but finding it before it is large enough to be felt is not?"