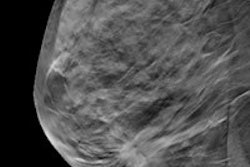
Whole-breast ultrasound (WBUS) is still a valuable adjunct to conventional mammography, even if digital breast tomosynthesis (DBT) is available, according to Yale University researchers, who discovered that WBUS found some cancers that DBT missed.
When added to conventional mammography, both WBUS and DBT can increase the cancer detection rate of breast screening. But there are still some invasive cancers that tomosynthesis misses -- and ultrasound can find these, said Dr. Regina Hooley, who presented the research at the RSNA 2013 meeting.
Hooley and colleagues investigated the performance of WBUS in women who had a recent normal breast tomosynthesis exam.
"Screening breast ultrasound is being more widely performed, primarily due to breast density notification laws," she told session attendees. "Because dense breast tissue can mask an underlying tumor, the false-negative rate of mammography in patients with dense breast tissue is higher compared to women without dense breast tissue."
 Dr. Regina Hooley from Yale University.
Dr. Regina Hooley from Yale University.
When used with mammography, breast ultrasound's supplemental cancer detection rate is three to four cancers per 1,000 women screened; on the other hand, the supplemental cancer detection rate of digital breast tomosynthesis in combination with mammography is 0.5 to 2.7 cancers per 1,000 women screened, Hooley said.
The study included 1,046 women who underwent handheld WBUS between October 2011 and September 2012 for screening because they had dense breast tissue. Each of the women also had a prior normal DBT mammogram performed within 12 months before the WBUS examination. Scans were performed on a commercially available ultrasound scanner (iU22, Philips Healthcare).
All of the ultrasound exams were performed according to the American College of Radiology Imaging Network (ACRIN) 6666 trial's ultrasound screening protocol by experienced technologists, and they were read by one of eight board-certified, fellowship-trained mammographers, Hooley said. The interpreting radiologists had access to the results of the patient's prior mammogram and the option to immediately image the patient again themselves with ultrasound if there was a questionable or positive finding.
The average age of the patients was 52 years, and the average time between the conventional mammogram and the ultrasound was about a month. Forty-three percent of the cases included in the study were incident exams, and 57% were prevalence exams, Hooley said.
Of the 1,046 cases, 911 (87.1%) were BI-RADS 1 or 2, 104 (9.9%) were BI-RADS 3, and 31 (3%) were BI-RADS 4. There were no BI-RADS 5 lesions. Thirty-one women underwent ultrasound-guided aspiration or biopsy. Two BI-RADS 4 lesions were malignant infiltrating ductal carcinomas, and neither was seen on DBT, even in retrospect. The overall positive predictive value for BI-RADS 4 lesions was 6.5%. The cancer detection rate was 1.9 per 1,000 exams.
Of the women included in the study, 71% had a one-year follow-up mammogram, while 57% had a one-year follow-up ultrasound. No interval breast cancers were found.
"We know that using screening ultrasound or DBT with full-field digital mammography increases the cancer detection rate, compared to full-field digital mammography alone, although ultrasound is offered primarily to women with dense breasts," Hooley said. "DBT-occult, screening ultrasound-detected cancers do exist."
Supplemental screening ultrasound performed in addition to DBT can detect mammographically occult breast cancers, although the rate is lower than in previous studies of screening ultrasound performed in addition to conventional digital mammography, Hooley concluded.
"More studies are needed to determine the long-term benefit of supplemental WBUS in women receiving DBT," she told session attendees.