VIENNA - The fifth edition of the BI-RADS atlas has been released, and while there have been several changes, perhaps the most important is the uncoupling of the assessment category and management recommendation, according to presenters at an ECR 2014 session on Sunday afternoon.
It's been more than 10 years since the last BI-RADS edition came out. In this edition, released by the American College of Radiology (ACR) in February, radiologists are no longer shoehorned into management options. This is particularly useful for BI-RADS 3, easily the most troublesome category. For probably benign lesions, radiologists can now add additional information and specify, for instance, whether a biopsy should be conducted based on clinical circumstances.
"Sometimes you'll have a probably benign lesion where you decide to do biopsy, and in the old days you would have to decide whether you would raise the BI-RADS category into category 4 to be able to biopsy it," said Dr. Ulrich Bick, a radiology professor and vice chairman in the radiology department at Charité University in Berlin, who presented changes to the BI-RADS atlas on mammography. "Now you still call it probably benign but have a management recommendation based on some additional information that you want to biopsy it."
Other differences in the mammography section include how dense tissue is named. In the old BI-RADS edition, breast composition was segregated into categories 1 through 4. In the new edition, breast composition categories are A, B, C, or D. "A" is entirely fatty and "D" is extremely dense.
In addition to changes in the nomenclature, radiologists may also omit the specific percent density (i.e., 25%, 50%, or 75%). The density categories depend on the densest part of the mammogram, so even if the mammogram is more than 50% fatty, if it has a very dense area behind the nipple, the breast would be categorized as C or maybe D, but the percentages do not have to be specified, according to Bick.
Radiologists are encouraged to describe regional differences where cancer is likely to be missed and where additional ultrasound may be helpful, he said. The emphasis is on the masking effect of dense fibroglandular tissue of mammographic depiction on calcified lesions and is not meant as a predictor of breast cancer risk.
Another big change is that suspicious calcifications are no longer separated into intermediate concern and higher probability of malignancy.
"All calcifications need the same management: biopsy; it doesn't matter if they're higher or lower probability of malignancy, they're all clearly above the threshold of 2% and you need tissue diagnosis," he said.
There are other small changes in the new BI-RADS edition -- "cleanup," Bick calls them -- including changing the term "isodense" to "equal density." "Lobulated" to describe shape was also removed because it was confused with margin characteristics, so now the options are only oval, round, or regular.
Mammography was not the only section to be altered; ultrasound and MRI experienced some changes too.
For ultrasound, there were updates in lexicon descriptors such as masses, calcifications, associated features (now constituting surrounding tissue with stiffness assessment), and special cases.
There is also guidance on how to link BI-RADS descriptors with management recommendations.
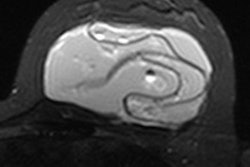
For breast MRI, the changes were also primarily "cleanup." For instance, nonmass-like enhancement has been changed to nonmass enhancement and internal enhancement characteristics no longer include central enhancement and enhancing septa.
There is also a section on implant assessment: whether they're saline or silicone, subpectoral or pectoral, etc.
The new edition is a hefty tome: "It weighs 4 kg [9 lb]," Bick said. "I brought it to ECR and it was so heavy the airline almost didn't let me carry it on."