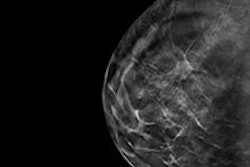
CHICAGO - Patients recalled from screening with full-field digital mammography (FFDM) plus digital breast tomosynthesis (DBT) do not all benefit equally from additional mammography for diagnostic evaluation, according to a presentation given on Wednesday at RSNA 2014.
Using follow-up mammography more appropriately could also spare women additional radiation exposure, save money, and make a busy department's operations more efficient, the researchers noted.
 Dr. Richard Sharpe of Beth Israel Deaconess Medical Center.
Dr. Richard Sharpe of Beth Israel Deaconess Medical Center."Conventionally, patients recalled from screening with tomosynthesis undergo additional imaging workup with digital mammography as the next step, rather than ultrasound," said presenter Dr. Richard Sharpe of Beth Israel Deaconess Medical Center. "We wanted to investigate whether additional mammography is actually helpful for working up abnormalities found on screening DBT."
Sharpe and colleagues culled data from 5,342 FFDM plus DBT exams performed between December 2012 and February 2014. Of these, 323 were interpreted as BI-RADS 0 (additional imaging needed), and 351 abnormal findings were identified. When patients returned for diagnostic follow-up -- whether with mammography, ultrasound, or both -- the interpreting radiologist noted whether mammography provided clinically useful information about screen-detected abnormalities beyond what was available from the original tomosynthesis exam.
Of the 351 abnormal findings, 183 were masses (52.1%), 75 were asymmetries (21.4%), 75 were calcifications (21.4%), and 18 were architectural distortions (5.1%).
Additional mammographic imaging was helpful almost half the time, for 170 of the 351 abnormalities (48.4%), Sharpe and colleagues found. But it helped in particular with calcifications, he said.
"For calcifications, mammographic follow-up imaging was helpful 92% of the time," he said.
For masses, additional mammography was helpful 24.6% of the time, while it helped 62.2% of the time for asymmetries and 55.6% of the time for architectural distortions.
As for the study's limitations, Sharpe acknowledged that he and his team do not yet have outcomes data that would definitively evaluate follow-up mammography's usefulness. And he conceded that radiologists might define "useful" differently.
"There aren't clearly defined criteria as to what is useful and what isn't -- that's left up to the individual radiologist," he said.
But the study takeaway is that the value of using additional diagnostic mammography varies by lesion type, Sharpe concluded.
"Our study suggests additional diagnostic mammography should be performed in evaluating microcalcifications, but it may not be necessary for evaluation of masses, asymmetries, and architectural distortion seen on screening DBT," he told session attendees. "And if diagnostic mammography could be avoided, there is potential to increase patient satisfaction, decrease patient radiation exposure, lower costs, and improve operational efficiency."