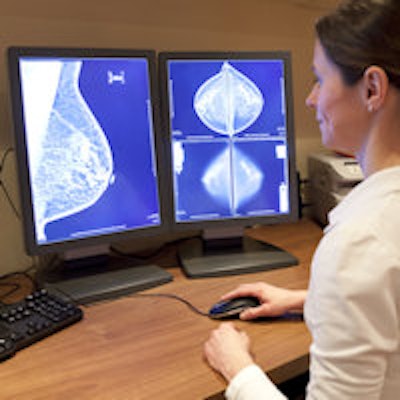
How can the quality of mammography interpretation be improved? That question was the subject of a workshop convened by the Institute of Medicine (IOM) earlier this month in Washington, DC. The meeting indicates that mammography quality remains a vexing issue, 10 years after the U.S. Congress reauthorized the Mammography Quality Standards Act (MQSA).
At the May 12 workshop, hosted by IOM's National Cancer Policy Forum and sponsored by the American Cancer Society (ACS), participants reviewed current evidence on interpretation performance in mammography and considered potential opportunities for advancing research and practice.
"There have been a lot of innovations in breast imaging since the MQSA was first instated," Dr. Patricia Ganz, vice chair of the National Cancer Policy Forum and a professor at the University of California, Los Angeles, told AuntMinnie.com. "This workshop provided a platform for discussing what has changed."
Ways to improve mammography
In 2005, in preparation for reapproval of MQSA, Congress asked IOM to produce a report that would recommend ways to improve the quality of mammography, with an emphasis on physician interpretation. That document, called "Improving Breast Imaging Quality Standards," emphasized the need to decrease variability in mammography interpretation in the U.S. and identified gaps in the evidence required to develop best practices.
Since then, new research about mammography interpretation has been published, including an assessment of factors that influence interpretive performance. Workshop participants explored questions about the minimum volume necessary for high-quality mammography interpretation, whether tests can be used to identify radiologists performing below minimum standards, and whether live instructor-led or self-paced interventions could be used to improve interpretive performance.
"The MQSA has had the effect of putting mammography performance under a microscope, and it's clear that we've still got a ways to go in terms of decreasing interpretation variability," workshop committee planning chair Diana Buist, PhD, from the Group Health Research Institute in Seattle, told AuntMinnie.com.
Experts weigh in
The meeting gathered representatives from ACS and the U.S. Food and Drug Administration's (FDA) MQSA program, along with a number of leaders from the American College of Radiology (ACR):
- Dr. Carl D'Orsi, of Emory University and chair of ACR's Committee on BI-RADS, spoke about the challenges of delivering high-quality mammography.
- Dr. Debra Monticciolo, of Texas A&M College of Medicine and chair of ACR's Commission on Quality and Safety, addressed the effects of training and experience on interpretive performance.
- Dr. Etta Pisano, of the Medical University of South Carolina and principal investigator of the ACR Imaging Network (ACRIN) Digital Mammography Imaging Screening Trial, presented an overview of IOM's 2005 report.
Dr. Barbara Monsees, from Washington University in St. Louis, discussed current challenges to breast imaging and cautioned attendees that there are still issues that need to be resolved, even though mammography quality has gotten better and advances such as digital breast tomosynthesis can improve screening.
"Expectations for breast imaging are high," she said. "Medicolegal implications are an issue. Variability in interpretation has been a problem, and double reading is not feasible. And although there are more modalities and procedures that can be helpful in patient management, these can be time-consuming."
Another issue that came to the fore was whether audits are effective for improving mammography interpretation performance. Audits have several limitations, said Robert Smith, PhD, director of cancer screening for ACS.
"General outcome measures tell us very little about areas that need improvement," he said. "It can take several years for poor interpretive performance to be identified. And it can take several years to measure improvement after corrective action has been taken."
So what are some ways mammography interpretation could be improved? Smith gave a number of suggestions:
- Invest in the next generation of breast imagers by creating curricula that include an emphasis on the value of audits, benchmarks, self-assessment, and feedback.
- Make continuing medical education requirements for mammography more rigorous.
- Create a more meaningful MQSA-mandated audit process by separating screening and diagnostic exams.
- Link cancer registry data to mammography facilities.
- Address U.S. mammogram volume reading requirements -- perhaps by increasing them.
"Breast imaging centers need to facilitate feedback and adapt to new strategies that are associated with improved performance -- and reward quality performance," Smith said.
Future direction?
It remains to be seen whether the workshop will translate into changes in MQSA or result in another IOM report, Ganz told AuntMinnie.com.
"There's a chance that this workshop could lend impetus to another consensus study, and not just about mammography, but about screening practice in general," she said. "This workshop was timely because it fits into a larger context of a cancer screening and treatment quality agenda."