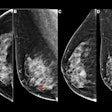
Digital breast tomosynthesis (DBT) has been getting positive press lately, with studies suggesting that it finds more cancers and reduces recall rates. So how can a facility best incorporate DBT into its practice? There are a few key considerations to take into account, according to a presentation at the Society of Breast Imaging (SBI) show in Austin, TX.
Facilities seeking to implement breast tomosynthesis need to carefully consider which vendor to work with, develop a strategy for integrating the technology into their department's workflow, and determine how to get the word out to patients and referring physicians that DBT is available, presenter Dr. Steven Poplack from Washington University School of Medicine and the Mallinckrodt Institute of Radiology, both in St. Louis, told session attendees.
Poplack has tomosynthesis chops: He was part of a team at Dartmouth-Hitchcock Medical Center in Lebanon, NH, that used the first Hologic DBT prototype in a 2004 multicenter reader study that led to premarket approval for the device. Dartmouth implemented screening DBT in February 2012; Mallinckrodt began using the technology for diagnostic exams that same year and has been using it for screening since 2013, Poplack said. Both institutions phased the technology in over time to minimize hassle and maximize benefit.
Pick your device
Currently, three vendors have breast tomosynthesis units that have been cleared by the U.S. Food and Drug Administration (FDA):
- Hologic's Dimensions was approved in February 2011; Dimensions with C-View (synthesized 2D images) was approved in May 2013.
- GE Healthcare's SenoClaire was approved in August 2014.
- Siemens Healthcare's Mammomat Inspiration was approved in April 2015.
Future DBT vendors will likely include Fujifilm Medical Systems USA and Philips Healthcare, Poplack said.
Each vendor's device has slightly different specifications, so facilities looking to install DBT should consider their options, he said.
| DBT system specifications by vendor | |||
| Hologic | GE Healthcare | Siemens Healthcare | |
| Device | Selenia Dimensions | SenoClaire | Inspiration |
| Detector | Amorphous selenium | Amorphous silicon | Amorphous selenium |
| Exposures | 15 low-dose exposures, 15° arc | 9 low-dose exposures, 25° arc | 25 low-dose exposures, 50° arc |
| Resolution | 70 microns (digital mammography); 95 (DBT) | 100 microns (for both digital mammography and DBT) | 85 microns (for both digital mammography and DBT) |
| Reconstruction | Filtered back projection | Iterative | Filtered back projection |
How to implement?
A facility can integrate DBT into its practice either with a complete conversion that swaps out all the old units with new systems, or with a more limited installation that replaces only some of the existing units, Poplack said.
"There's no 'right way' to implement DBT," he told AuntMinnie.com. "Implementation depends on what makes the most sense for each practice."
Dartmouth-Hitchcock underwent a three-phase implementation. Phase 1 consisted of a single DBT unit in the facility's screening center; patients were triaged based on whether they or their provider requested DBT, as well as their baseline mammograms. Women with dense tissue are also good candidates.
In phase 2, Dartmouth acquired a second unit for diagnostic purposes, and in phase 3 the institution installed a DBT device for guided large-core needle biopsy.
"Dartmouth's three-phase, partial implementation was determined by the capital resources we had," Poplack said. "The choice to begin with screening was based on the belief that screening provided the greatest benefit to women."
Mallinckrodt Institute of Radiology also underwent a phased implementation, with diagnostic tomosynthesis implemented in March 2012 and screening tomosynthesis in December 2013 -- but the institution replaced all of its digital mammography units at each phase.
There was no patient triage, although some patients were excluded, such as women with very large breasts, those with pacemakers or implants, patients older than 75, or those with comorbidities that might compromise image quality due to longer acquisition times, Poplack said.
Market your services
Once you've selected a DBT device, it's important to consider how to market the service -- not only to patients, but also to referring physicians, Poplack told the SBI 2016 attendees.
"Inform your medical staff and requesting providers that you have DBT through grand rounds, especially for primary care services such as family practice, ob/gyn, and internal medicine," he said. "And make use of your hospital's system-wide email or even a newsletter."
Optimize your website so that patients can find information about DBT easily, and consider using radio, newspaper, or television ads to get the word out as well. Finally, create a fact-sheet pamphlet and/or a poster for the waiting room, Poplack said.
"Educate all your staff so they can help get the word out," he said.
A few practical considerations
Finally, if a facility is planning the transition to DBT, it's important to think about a few practical aspects of the change, such as a learning curve for interpretation times, Poplack said. When radiologists start using the technology, they do tend to take more time to read tomo images until they become more familiar with them.
"Figure that in the beginning, interpretation time for digital mammography plus DBT will be twice that of digital mammography alone," he said.
What are some other things to consider? Integrate DBT into your pre-existing digital mammography protocol, and create a reading room environment that mitigates distraction. Think about setting volume limits -- perhaps batch reading of no more than 20 DBT exams at a time.
"Some experienced DBT users advocate for reading digital mammography images first, then using DBT images to evaluate possible recalls and to scan for hidden digital mammography findings," Poplack said.
Finally, add DBT to the department's electronic order-entry options, make sure referring physicians are notified when the exam has been performed, and set up billing codes that differentiate DBT exams from digital mammography. And don't forget to consider whether more staff, storage, and network resources will be needed.
In any case, offering DBT to patients is sound medicine, Poplack said.
"You can feel good that your practice is providing patients with a better mammogram," he concluded.