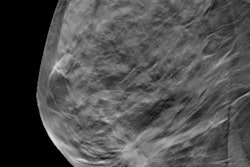
Synthetic 2D mammograms received the thumbs up for breast cancer screening from researchers at the Hospital of the University of Pennsylvania (HUP) in a July 28 article published in Radiology. They say the exams are good enough to replace conventional digital mammography studies as a complement to digital breast tomosynthesis (DBT).
The HUP researchers screened more than 5,300 women with a combination of DBT and synthetic 2D mammography. Compared with DBT and conventional digital mammography, the synthetic studies had a lower recall rate and 39% lower radiation dose, with no statistically significant difference in cancer detection rate.
"Synthetic 2D certainly is an attractive way to hopefully cut the dose of the study, because the woman is only receiving the dose from the tomosynthesis acquisition," said Dr. Emily Conant, one of the co-authors of the study (Radiology, July 28, 2016).
A thorny problem
Synthetic 2D mammography is a possible solution to a problem created by the rise of DBT for screening. Because tomosynthesis is a 3D modality, sites using DBT for screening have also had to acquire conventional planar 2D digital mammography studies. This leads to higher radiation dose for women, a particularly thorny issue when women could receive multiple screening exams over their lifetimes.
 Dr. Emily Conant from the University of Pennsylvania.
Dr. Emily Conant from the University of Pennsylvania.This problem is potentially solved by synthetic 2D mammography, in which a "synthetic" 2D exam is created from the 3D slices produced by the DBT study. This can reduce radiation dose by up to 45%, according to previous studies.
But how well does synthetic 2D in combination with DBT perform from a clinical standpoint? Recent clinical results have been encouraging. A June 23 paper in Lancet Oncology found that the combination had an equivalent cancer rate to DBT with conventional mammography. A study presented at the Society of Breast Imaging conference in April 2016 also was positive.
As early adopters of screening with synthetic 2D exams, the HUP researchers decided to analyze data acquired at their facility with a combination of DBT and synthetic 2D exams, and compare the results with screening with DBT and conventional digital mammography. They first presented a paper on their findings at RSNA 2015, and since then they have added data from more patients.
In the Radiology paper, the researchers present data on 5,366 women who were screened between January and June 2015 with DBT and synthetic 2D mammography, as well as 15,571 women who received DBT and conventional digital mammography. All women from both groups were screened with a commercially available mammography system capable of 2D synthetic mammography (Selenia Dimensions, Hologic).
The primary outcomes included cancer detection rate, biopsy rate, radiation dose, recall rate for clinical issues such as suspicious lesions, and recall rate for technical issues such as poor positioning or patient motion. The researchers also tracked patient demographic factors such as breast density.
When the numbers came in, there was no statistically significant difference in the cancer detection rate between DBT with synthetic 2D images and DBT with conventional mammography. In addition, the synthetic technique had the edge in a number of different areas, while delivering radiation dose that was 39% lower.
| Screening with DBT + synthetic 2D vs. DBT + conventional mammography | |||
| DBT + synthetic 2D mammography | DBT + conventional mammography | p-value | |
| Cancers detected per 1,000 screened | 5.03 | 5.45 | 0.723 |
| Clinical recall rate | 7.1% | 8.8% | < 0.001 |
| Technical recall rate | 0.1% | 0.2% | 0.03 |
| Biopsy rate | 1.3% | 2.0% | 0.001 |
| Invasive cancers vs. ductal carcinomas in situ per 1,000 screened | 4.10 | 3.85 | 0.301 |
| Radiation dose | 4.88 mGy | 7.97 mGy | < 0.001 |
There was no statistically significant difference in the proportion of invasive cancers versus ductal carcinomas in situ (DCIS) detected by synthetic 2D mammography and DBT compared to DBT with conventional mammography.
A vote of confidence
The data represent a welcome vote of confidence in synthetic 2D mammography from a site that might have the most clinical experience with it. HUP converted its screening population to synthetic 2D mammography in January 2015, and HUP's university-based site continues to screen with the synthetic technique, Conant told AuntMinnie.com.
A major benefit that HUP enjoyed was that it had a four-month period in which synthetic 2D screening overlapped with conventional mammography. This helped HUP's breast imagers get used to the appearance of synthetic 2D mammograms, which can differ from that of conventional 2D mammography studies. Conant recommends that sites adopting the synthetic technique build in a similar transition period.
"Our readers could get used to the appearance of the synthetic image and have the 2D regular mammogram to turn to if there were differences in the appearance of the breast and potentially of lesions," she said. "Definitely there should be an overlap period where all the radiologists get exposed to both 2D and synthetic images. They can begin to understand the specifics of the appearance of the breast, by thickness, density, and lesion subtype."
Conant believes that synthetic 2D mammography will continue to improve with better data reconstruction algorithms. At HUP, the researchers are looking forward to continuing their work, especially after analyzing a full year of data, from January 2015 to January 2016. They also plan to further study synthetic 2D mammography's rate of invasive cancer detection versus DCIS detection, as well as false negatives that might have been missed by the technology.
"I do very much believe that synthetic imaging is the way to go with tomosynthesis to answer the 2D task that radiologists need to address, the things we look at in a mammogram that are 2D tasks," Conant said. "We need the synthetic image, and I believe it is going to get even better over time."