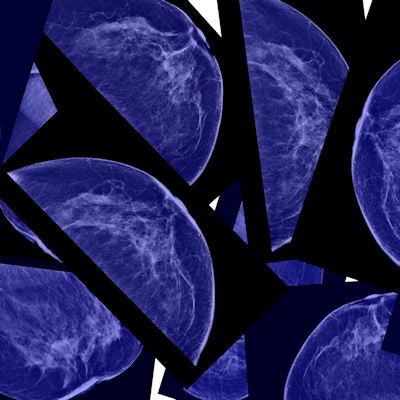
Screening digital breast tomosynthesis (DBT) has been shown to reduce recall rates, increase cancer detection, and identify more invasive cancers. But does it also boost short-term follow-up rates? Researchers sought to answer this question in a study published online December 2 in Academic Radiology.
A team led by Dr. Jaclynn Powell of Ohio State University found that women who underwent DBT were 80% more likely to receive a BI-RADS 3 recommendation than women who underwent digital mammography alone -- a lesion category that tends to prompt a short-term follow-up protocol. Higher rates of short-term follow-up are a concern because they could lead to women being seen again for findings that ultimately turn out to be benign, and even increase the number of false-positive biopsy recommendations (Acad Radiol, December 2, 2016).
 Dr. Jaclynn Powell of Ohio State University.
Dr. Jaclynn Powell of Ohio State University."A potential drawback to [DBT's] increased conspicuity of some lesions in dense breasts, particularly in young women, is an accompanying increase in the detection of benign lesions that would otherwise be obscured [on digital mammography] by overlapping breast tissue," the authors wrote. "This could prompt further workup and possibly result in higher rates of short-term follow-up for probably benign findings."
However, it is possible that increased short-term follow-up rates are simply part of the process for implementing DBT in a practice, Powell told AuntMinnie.com.
"This trend could be part of the learning curve for radiologists when DBT is implemented," she said. "We find things that might have been there for years. But as we continue to use the technology, we get better at discerning which findings don't necessarily need follow-up."
Beware of BI-RADS 3?
For the study, Powell's group included 12,781 screening mammograms performed between June 2012 and August 2014. Of these, 10,477 were acquired with digital mammography and 2,304 were acquired with digital mammograms plus tomosynthesis. Of the women who underwent digital mammography only, 1,694 were recalled for further imaging; meanwhile, 318 of those who had combination exams were recalled.
The researchers tracked the women's clinical, imaging, and pathologic features, including patient age, availability of prior mammograms, and breast density, as well as presence of invasive cancer, ductal carcinoma in situ (DCIS), or benign lesions.
DBT reduced the overall recall rate by 12.5% and improved the positive predictive value for recall (PPV1) by 47%, compared with digital mammography alone. It also improved the PPV2 (cancers per biopsies recommended) and PPV3 (cancers per biopsies performed) rates, but these results were not statistically significant.
| Comparison of clinical performance: Digital mammography and DBT | |||
| Measure | Digital mammography | DBT + digital mammography | p-value |
| Recall rate | 16% | 14% | 0.017 |
| Cancers per 1,000 women screened | 5.2 | 7.8 | -- |
| PPV1 (cancers per recalls) | 3% | 5.6% | 0.032 |
| PPV2 (cancers per biopsies recommended) | 25.1% | 29.5% | 0.689 |
| PPV3 (cancers per biopsies performed) | 25.3% | 29.5% | 0.516 |
| Short-term follow-up rate per 1,000 women screened | 36 | 44 | 0.072 |
In the group of patients who underwent digital mammography only, 61% of cancers were invasive and 39% were DCIS; in the digital mammography plus DBT group, 44% of cancers were invasive and 56% were DCIS, the researchers found.
The most concerning finding was a trend toward increased short-term follow-up in the DBT group versus the digital mammography group, with 44 per 1,000 screens versus 36 per 1,000 screens (although the difference was not statistically significant), according to the researchers. In fact, after adjusting for patient age, breast density, and absence of prior mammograms, they found that the likelihood of a BI-RADS 3 recommendation was 80% higher in the DBT group than in the digital mammography group.
Powell and colleagues noted that one of the study's limitations was its small sample size for DBT exams, and that further studies are needed.
"Further studies are needed to determine the malignancy rate of BI-RADS 3 lesions detected at DBT screening and to determine appropriate follow-up to maximize cancer detection while minimizing patient expense and anxiety," they wrote.
In any case, this study affirms DBT's benefits, and as the technology continues to be incorporated into more radiology practices, it's only a matter of time before the issue of higher short-term follow-up rates is addressed, according to Powell.
"Our study confirms the many benefits of DBT, including decreased recall rates and improved PPV1," she said. "As it continues to be used more widely, we would expect to see this trend of increased rates of short-term follow-up to resolve."