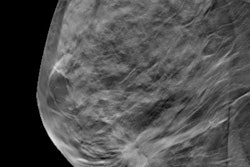
Digital breast tomosynthesis (DBT) has been shown to reduce recall rates and increase cancer detection in screening when compared with digital mammography. But are these improved performance metrics sustained over time? Two researchers addressed this question at the recent RSNA 2016 meeting in Chicago.
Researchers led by Dr. Christine Chen from Yale University reviewed DBT exams performed over four consecutive years (August 2011 to July 2015). They analyzed the recall rate, cancer detection rate, and positive predictive value for recall (PPV1) for each one-year period and compared the results with those from a control group of digital mammography exams taken between August 2008 and July 2010.
The analysis included 42,470 screening DBT exams over the four-year period and 20,533 digital mammography exams over the two-year period.
| Performance over time: DBT vs. digital mammography | |||||
| Metric | DBT Year | 2D mammo (2-year average) | |||
| 1 | 2 | 3 | 4 | ||
| Recall rate | 7.9% | 8.7% | 7.9% | 7.5% | 11.4% |
| Cancer detection rate (per 1,000 exams) | 5.7 | 5.1 | 5.9 | 6.4 | 3.8 |
| PPV1 | 7.2% | 5.9% | 7.4% | 8.5% | 3.4% |
| Percent of invasive cancers found | 50% | 55% | 59% | 74% | 59% |
DBT's recall rates were significantly reduced over the study duration, compared with digital mammography (p < 0.0001). The increase in cancer detection rate for DBT was statistically significant, compared with 2D mammography, in the third and fourth DBT years (p < 0.05). In addition, DBT's increased PPV1 was statistically significant across the second through fourth DBT years (p < 0.05).
The study findings show a trend of steady improvement in DBT's outcome metrics over time, according to Chen.
"The sustainable, superior performance of DBT over [digital mammography] illustrates the integral role of DBT in breast cancer screening, which has important implications for policymaking in the future," she concluded.
Mixed results?
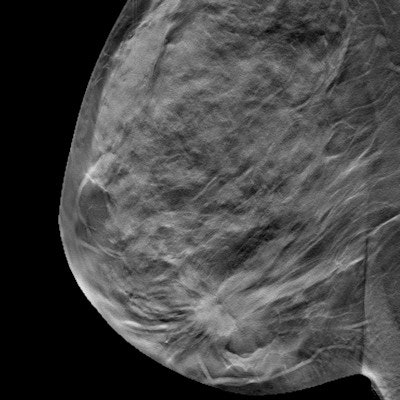
In a related study, a team led by Dr. Pragya Dang from Massachusetts General Hospital sought to compare DBT's screening performance with that of digital mammography alone.
The researchers identified consecutive screening DBT exams taken between January 2013 and March 2015, and consecutive screening mammography exams taken between January 2009 and March 2011. They calculated the abnormal interpretation rate, the cancer detection rate, and the positive predictive value of each technology, adjusting for patient demographics.
The study included 76,987 DBT exams and 78,298 digital mammography exams. Dang's group found the following:
- The abnormal interpretation rate of the DBT group was lower than in the digital mammography group, at 6.26 versus 6.89 (p < 0.0001).
- The cancer detection rate for DBT did not differ significantly from the rate for digital mammography, at 4.9 per 1,000 screens versus 4.7 per 1,000 screens (p = 0.74).
- PPV1 (positive predictive value for recall) was 7.8% for DBT and 6.6% for digital mammography.
- PPV2 (cancers per biopsies recommended) was 36.4% for DBT and 34.8% for digital mammography.
- PPV3 (cancers per biopsies performed) was 41.1% for DBT and 40.7% for digital mammography.
The findings may give practices that are just beginning to use tomosynthesis a better sense of the implementation process.
"The benefit of reduced false positives with implementation of tomosynthesis is sustained over time," Dang said. "However, increased cancer detection rates ... may not persist in established tomosynthesis practices."