Presenting information to men and women about the "harms" of prostate and breast cancer screening significantly diminishes their interest in screening exams, according to a study published in the January/February edition of the Annals of Family Medicine.
After viewing a video that included information about the limits and harms of each respective screening test, as well as a printed decision aid, the number of men who said they wanted to be screened fell by 36 percentage points, while the number of women who said they wanted to be screened fell by 37 percentage points.
 Dr. Barry Saver of Swedish Family Medicine.
Dr. Barry Saver of Swedish Family Medicine."Americans receive substantial amounts of low-value medical care," wrote a group led by family practice physician Dr. Barry Saver of Swedish Family Medicine in Seattle. "When recommending against care can evoke fear and distrust, clinicians are challenged to explain why a test or treatment might not be beneficial, a challenge compounded by advocacy groups mounting campaigns based on strong, emotional messages rather than unbiased evidence."
Challenging cases
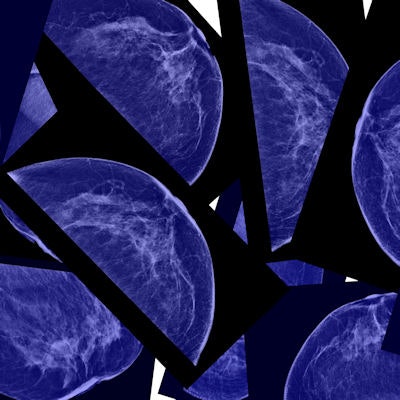
The study presents the results of an evaluation of interventions developed to help patients "consider and trust" the 2009 U.S. Preventive Services Task Force (USPSTF) recommendations on breast screening for women in their 40s, as well as the 2012 recommendations against prostate cancer screening, according to the authors (Ann Fam Med, January/February 2017, Vol. 15:1, pp. 48-55). With respect to breast screening, the USPSTF in 2009 withdrew its recommendation that women in their 40s be screened, advising them instead to make a decision on screening after consulting with their physicians.
"We wanted to take a couple of challenging cases -- prostate and mammography screening," Saver told AuntMinnie.com. "While the USPSTF isn't perfect, we trust them to be unbiased and to have done the best they could with the evidence they had, based on the Institute of Medicine's approach to creating trustworthy guidelines."
Saver and colleagues conducted the study in three phases, the first of which was an assessment of patient attitudes toward prostate and breast cancer screening via focus groups. The researchers found the following:
- Participants needed information about the limits and harms of a screening test, because without this information, considering not being screened didn't make sense.
- Participants were not aware of existing screening guidelines. They were also not familiar with the USPSTF.
- Discussing how guidelines are developed and their potential biases had no effect on participants' attitudes toward screening.
- The experiences of family and friends with cancer screening, diagnosis, and treatment had a powerful influence on participants' views about screening.
- Participants wanted to know if there was good evidence to support a decision not to screen.
In the second phase of the study, the researchers developed videos, framed as a conversation between a physician and a patient, for both prostate and breast cancer screening.
The third phase, which was the focus of the paper, included 27 men and 35 women, all of whom saw the video intervention and also received a printed decision-aid intervention, in random order. Each person was surveyed about screening intentions, perception of benefits and harms, and any conflict about his or her screening decision before and after being exposed to the materials.
Following the video, the number of men and women who wanted screening dropped dramatically.
| Effect of intervention video on screening preferences | ||
| Before video | After video | |
| Men who wanted prostate screening | 69% | 33% |
| Men who were unsure of prostate screening | 31% | 11% |
| Women who wanted breast screening | 86% | 49% |
| Women who were unsure of breast screening | 6% | 20% |
The researchers also noted the following:
- Men's preferences changed primarily from wanting screening to not wanting it, while women's preferences were more balanced between being unsure and not wanting screening.
- The interventions resulted in a significant decrease in men's intentions to discuss prostate cancer screening with their physicians.
- Women's desired frequency of mammography changed after being exposed to the material. At the beginning of the study, 54% of women were in favor of annual mammograms and 34% were in favor of biennial exams; after the interventions, 14% were in favor of annual mammograms and 60% were in favor of biennial exams.
"When we say to patients, 'You need colon cancer screening,' or 'You need a mammogram,' almost none of them says, 'What's the evidence?' " Saver told AuntMinnie.com. "But if we say, 'You may not need this screening exam,' they do want evidence."
Risky interventions?
The study echoes previous research that indicated giving patients information on the harms of screening reduces their enthusiasm for procedures. For example, an Australian group in 2015 found that giving patients a decision aid that included information about overdiagnosis reduced the percentage who wanted screening by 13 percentage points, from 87% to 74%.
The problem with research like the current study is that it's risky to use the USPSTF's guidance as a gold standard for screening protocols, according to Dr. Debra Monticciolo, chair of the American College of Radiology's (ACR) breast imaging commission.
"Regarding mammography screening, the task force has not had any breast imaging experts on its panel," she told AuntMinnie.com. "And if task force information is being presented as all the evidence, that's scary."
For example, the videos Saver's team developed don't reflect the full amount of evidence about mammography's benefits, Monticciolo said.
"Patients need accurate information about screening exams -- that's a given," she said. "And there's good science out there that supports screening protocols that doesn't make the news. The problem with a study like this is that it's a small pilot, and in terms of the mammography video [it] does not present the full range of evidence of breast cancer screening's benefits."
Monticciolo encourages radiologists to commit to making sure patients have accurate information about screening.
"My message to radiologists is to get involved with our patients and make sure they've got really good, accurate information about screening -- including the downsides," she said. "We can't give up. We have to continue to be proactive and advocate for our patients."