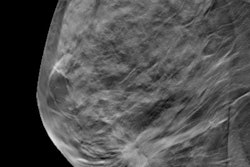
Although there are factors that can boost a woman's dose during a mammography exam, breast density isn't one of them, according to a study published June 7 in the Breast Journal. The findings are good news for women with dense tissue who may consider skipping mammography altogether, especially because density is known to affect the modality's efficacy.
Avoiding mammography because of dose concerns isn't necessary, wrote the team led by Dr. Jonathan Nguyen from the University of Virginia Health System in Charlottesville.
 Dr. Jonathan Nguyen from the University of Virginia Health System.
Dr. Jonathan Nguyen from the University of Virginia Health System."The results of our study demonstrate that breast density is a minor determinant of radiation dose from digital screening mammography, accounting for just 10% of the dose," the group wrote. "Women with dense breast tissue should not defer mammographic screening due to concerns about radiation dose."
Dose boosters
Women have become savvier about breast tissue density and how it affects mammography, due in part to the fact that many U.S. states have density notification laws in place that require women to be notified if they have dense tissue, Nguyen and colleagues wrote. Fear of undue radiation is certainly a valid concern, but it's important to understand the factors that actually increase dose at mammography, he told AuntMinnie.com.
"It's actually compressed breast thickness and body mass index that increase mammography's radiation dose the most," he said.
There hasn't been much published data about how density might affect dose, a situation that Nguyen's group sought to correct. The researchers evaluated the relative contribution of breast density to radiation dose by collecting data on patient age, weight, height, compressed breast thickness, and average glandular dose for 434 women who underwent screening mammography at the University of Virginia Health System in June 2014.
Median patient age was 58, and median body mass index (BMI) was 26.8. Median volumetric breast density was 5.8%, and median compressed breast thickness was 63.4 mm; median glandular dose was 1.68 mGy for the left breast and 1.75 mGy for the right breast. More than 70% of the women included in the study had fatty or scattered density breast tissue, the group wrote.
There was no association between increased dose and breast density, Nguyen and colleagues found; rather, it was breast thickness and BMI that increased radiation dose. In fact, compressed breast thickness accounted for 80% of the dose.
"Larger breast thickness results in larger overall attenuation, for which the system automatic exposure control compensates by the selection of a higher tube voltage (kVp) and/or current-time product settings," they wrote.
Patient education
The bottom line is that the majority of the radiation dose during screening mammography is driven by compressed breast thickness, and it's only minimally associated with breast tissue density. Therefore, women with dense tissue don't need to worry about increased dose, Nguyen and colleagues wrote. They hope that this research will help referring physicians discuss the benefits of mammography with patients.
"We hope that clinicians can use these findings to help address concerns women with dense tissue might have about radiation exposure at mammography," Nguyen told AuntMinnie.com.
Another takeaway? Good breast compression technique is important for minimizing radiation to the patient, according to Nguyen.
"Eighty percent of patient dose was affected by compression thickness," he said. "So one thing practices can do to reduce patient dose is urge their techs to get good compression."