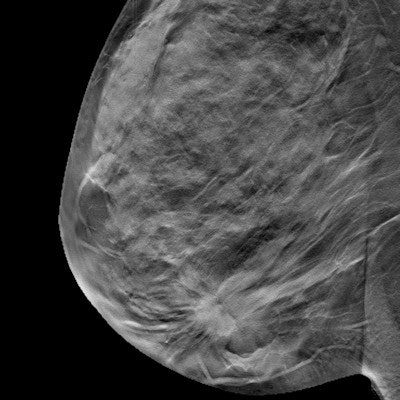
Adding digital breast tomosynthesis (DBT) to mammography when screening women in their 40s increases cancer detection rates and also decreases recall rates -- thus mitigating the "harms" that concern critics of screening in this age group, according to a study published online May 18 in Breast Cancer Research and Treatment.
Screening mammography has been shown to identify cancers at a smaller size and earlier stage, which improves a woman's prognosis; however, critics say that screening women in this age group doesn't make sense due to the lower incidence of cancer and potential harms such as false-positive recalls, wrote the team led by Dr. Elizabeth Rafferty of L&M Radiology in West Acton, MA.
 Dr. Elizabeth Rafferty of L&M Radiology.
Dr. Elizabeth Rafferty of L&M Radiology.But it may be that the debate is being driven by the wrong question, Rafferty told AuntMinnie.com. Rather than focusing on when screening should start, it would be better to ask how existing screening tools can be improved.
"The data bear out that women should begin breast cancer screening at age 40," she said. "What we need to do is refine the screening tools. Our study demonstrates that tomosynthesis is a great way to do that."
Superior screening?
Current screening guidelines vary, according to Rafferty and colleagues: The U.S. Preventive Services Task Force (USPSTF) recommends that women begin biennial screening at age 50, while the American Cancer Society (ACS) recommends annual screening starting at age 45 through age 55, with biennial screening thereafter. Other guidelines from societies such as the American College of Radiology (ACR) and Society of Breast Imaging (SBI) recommend annual screening starting at age 40.
The ACS guidelines are somewhat more nuanced, in that they recognize that clinical data do support beginning screening at a younger age, and they point toward improving the technology, Rafferty and colleague wrote.
"Following a comprehensive review of the evidence regarding mammographic screening, the ACS acknowledged the weight of existing evidence that mammography screening is associated with a significant reduction in breast cancer mortality after age 40 and suggested that subsequent efforts focus on improving the performance of mammography screening in order to shift the harm-benefit equation," they wrote.
To tackle this issue, Rafferty's group investigated the effect of adding tomosynthesis to digital mammography on breast cancer screening performance, specifically parsing the results by patient age.
The researchers compared screening performance metrics from 12 months before tomosynthesis was implemented to metrics gathered from a second period after tomo began to be used (range, 3-22 months). Patients were categorized in 10-year cohorts, starting at age 40. The study included 278,908 women screened with mammography alone and 173,414 screened with both mammography and DBT; the researchers calculated rates per 1,000 screens for recalls, cancers, and invasive cancers detected, as well as the positive predictive value for recall and positive biopsy rate.
Adding tomosynthesis to digital mammography resulted in significant reductions in recall rates for all age groups, but the largest reduction was for women between the ages of 40 and 49, decreasing the recall rate from 137 per 1,000 screens to 115, Rafferty and colleagues found. Tomosynthesis also improved the cancer detection rate in this age group (from 2.9 per 1,000 screens to 3.8), as well as the invasive cancer detection rate (from 1.6 per 1,000 screens to 2.7). These results were not affected by study participants' breast density, they wrote.
| Performance of full-field digital mammography (FFDM) vs. tomo + FFDM by age | |||||
| Performance measures | FFDM | FFDM + DBT | |||
| Recalls per 1,000 screens | |||||
| 40-49 | 137 | 115 | |||
| 50-59 | 102 | 89 | |||
| 60-69 | 89 | 77 | |||
| 70+ | 78 | 70 | |||
| Cancer detected per 1,000 screens | |||||
| 40-49 | 2.9 | 3.8 | |||
| 50-59 | 3.6 | 5 | |||
| 60-69 | 5.7 | 7.4 | |||
| 70+ | 7 | 8.2 | |||
| Invasive cancers per 1,000 screens | |||||
| 40-49 | 1.6 | 2.7 | |||
| 50-59 | 2.4 | 3.7 | |||
| 60-69 | 4.1 | 5.8 | |||
| 70+ | 5.2 | 6.4 | |||
| Positive predictive value for recall (PPV1) | |||||
| 40-49 | 2.3% | 3.4% | |||
| 50-59 | 3.8% | 6% | |||
| 60-69 | 6.9% | 10.3% | |||
| 70+ | 9.6% | 12.6% | |||
| Positive biopsy rate (PPV3) | |||||
| 40-49 | 13.7% | 17.6% | |||
| 50-59 | 21.9% | 26.3% | |||
| 60-69 | 35% | 39.2% | |||
| 70+ | 45.1% | 43% | |||
The fact that screening women in their 40s with DBT and digital mammography achieved the same level of performance as screening women in their 50s with full-field digital mammography alone makes a strong case for starting screening at 40 -- with tomosynthesis, according to Rafferty and colleagues.
"The magnitude of performance gains was greatest for women ages 40 to 49 and argues strongly for tomosynthesis screening for breast cancer detection as the standard of care for women beginning at the age of 40," they wrote.
Harm-benefit balance
The combined increase in cancer detection and reduction in false-positive examinations seen in women in their 40s with the addition of tomosynthesis to digital mammography shifts the balance of benefits versus perceived harms for women in this age group, the authors wrote.
"The consistent coupled effect of increased cancer detection and reduced false-positive findings in the delineated age subgroups affirms that digital mammography in combination with tomosynthesis represents an improved method of mammographic screening than digital mammography alone for women 40 and older," they concluded.