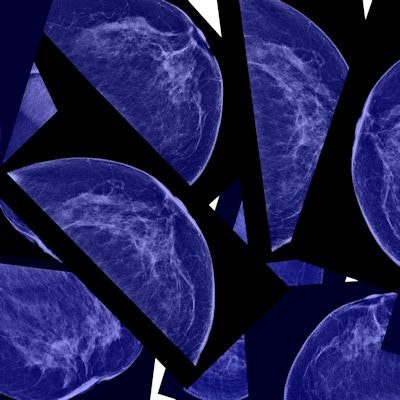
Screening with digital breast tomosynthesis (DBT) doesn't increase the use of BI-RADS category 3 -- a designation that prompts intensive follow-up and tracking for up to two years and can provoke anxiety in patients, according to a study published online July 17 in Radiology.
The findings are good news for women as practices continue to transition to DBT: Fewer BI-RADS 3 lesions translates into less uncertainty for women and potentially less healthcare costs due to additional imaging and biopsies, wrote a team led by Dr. Elizabeth McDonald, PhD, from the University of Pennsylvania.
"[Women with findings in the 'probably benign' category] are left to wait and wonder: When will resolution come, and what will be the ultimate outcome?" the authors wrote. "A decrease in this population could have substantial clinical and economic impact."
Less uncertainty
The BI-RADS 3 category allows physicians to track suspicious lesions for a time in the hope of avoiding biopsy, McDonald and colleagues wrote. Eventually, the lesion is established definitively as benign or, if a worrisome change is found, biopsy is recommended. But the fact that these lesions must be followed at six-month or one-year intervals can create anxiety that may affect a woman's willingness to comply with this continued screening.
"Patient compliance is known to decrease with each subsequent diagnostic examination, [which limits] the utility of the 'wait and see' approach," the authors wrote.
For the study, McDonald and colleagues included 10,728 screening digital mammography exams (taken between September 2010 and August 2011) and 15,571 screening digital mammography plus DBT exams (taken between October 2011 and February 2013). Recall rates were 10.4% for digital mammography and 8.8% for DBT plus mammography. The group also classified recall exams by finding type (calcifications, asymmetry or focal asymmetry, mass, and architectural distortion).
Although the researchers found no significant difference in the use of BI-RADS 3 in patients screened with mammography alone versus those screened with mammography plus DBT (1.6% vs. 1.3%, respectively), the overall number of women recommended for short-term follow-up fell by 2.4 women per 1,000.
That fewer women were recommended for short-term follow-up "is clinically meaningful considering the cost of additional imaging events, as well as the potential for anxiety associated with short-term follow-up," the group wrote.
McDonald and colleagues also found that there was no change between the two groups in the number of lesions categorized as BI-RADS 3 after diagnostic workup. Finally, they did discover that DBT's recall rate increased slightly for architectural distortions and decreased slightly for asymmetries.
"The increased recall of architectural distortion with DBT is ... expected due to [its] multiple projections and reconstruction, making both benign and malignant lesions more conspicuous," they wrote.
Minimizing harms
The study findings address one of "harms" of mammography: recalls, according to corresponding author Dr. Emily Conant, also of the University of Pennsylvania.
"There's so much interest right now in the so-called 'harms' or downsides of screening, and this study addresses one of them," she told AuntMinnie.com. "No one likes the BI-RADS 3 category -- radiologists hate it, and so do patients. So reducing the number of BI-RADS 3 lesions will help by reducing recommendations for short-term follow-up."