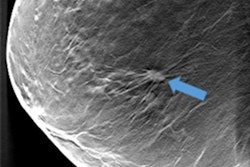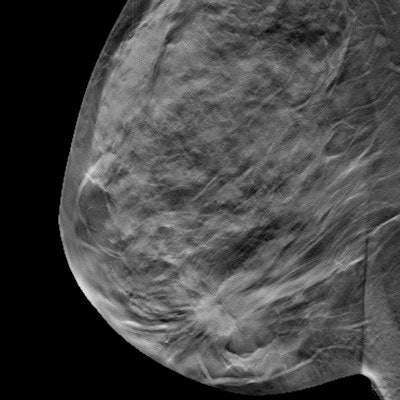
Screening with digital breast tomosynthesis (DBT) identifies smaller breast cancers with less axillary lymph node metastasis, compared with 2D screening mammography, according to research presented at the recent RSNA 2017 meeting in Chicago.
The finding indicates that the technology can improve outcomes for women diagnosed with early breast cancer.
"Our study suggests that, compared with digital mammography, DBT screening may improve breast cancer early detection, which may lead to less systemic treatment and improved clinical outcomes," said presenter Dr. Maryam Etesami of Yale University School of Medicine and the Smilow Cancer Hospital at Yale New Haven.
Smaller is better
Digital breast tomosynthesis has been shown to reduce false-positive recalls for screening mammography exams, while also increasing the cancer detection rate of screening when compared with conventional digital mammography. However, the tumor characteristics and clinical significance of cancers identified by DBT are not well-understood, Etesami said.
 Dr. Maryam Etesami from Yale University.
Dr. Maryam Etesami from Yale University."DBT is a relatively new technique in breast imaging, and available data on screen-detected cancers over several years of consecutive use is limited," she told session attendees.
To remedy this, she and her colleagues sought to identify cancer characteristics through a study that compared a total of eight years of DBT and digital mammography exams. The study included 44,050 screening mammograms: 15,768 (36%) were digital exams performed between August 2008 and August 2011, before DBT was installed at Yale, and 28,282 (64%) were combination 2D/DBT exams performed between August 2011 and August 2016.
Two standard views -- mediolateral oblique (MLO) and craniocaudal (CC) -- were acquired for each breast on 2D mammography; after DBT was installed, the 3D technique was offered to women at no additional cost, and the same two standard views were taken in a combination exam.
The researchers tracked the following screen-detected cancer characteristics:
- Invasive cancer versus ductal carcinoma in situ
- Histological type
- Histological differentiation
- Receptor phenotype
- Size
In terms of cancer detection, the overall rate between DBT and 2D mammography was not statistically significant: DBT found 153 cancers, for a detection rate of 5.41 per 1,000 patients, while 2D digital mammography found 78, for a detection rate of 4.95 per 1,000 patients.
There was no statistically significant difference in the percentage of invasive cancers detected (67% with DBT and 71% with digital mammography). In addition, the histological type, differentiation, or receptor phenotype of screen-detected cancers did not differ significantly between the two modalities.
But Etesami's team did find that the mean size of invasive cancers identified on DBT exams was smaller than the size found on digital mammography -- 1.4 cm compared with 1.8 cm -- and that DBT had fewer positive axillary lymph nodes compared with 2D mammography (15% versus 31%). Both these results were statistically significant.
| 2D mammography vs. DBT for breast cancer screening | ||
| 2D mammography | DBT | |
| Cancer detection rate per 1,000 patients | 4.95 | 5.41 |
| Invasive cancer size (mean) | 1.8 cm | 1.4 cm |
| Positive axillary lymph nodes | 31% | 15% |
"We were pleased to see that axillary lymph node metastasis in invasive cancers was reduced to approximately half with DBT screening compared to digital mammography-only screening," Etesami said.
Finally, the more clinically significant cancers -- that is, moderately or poorly differentiated invasive cancers -- detected by DBT had fewer positive axillary lymph nodes (20% with DBT versus 38% with 2D mammography).
"As we know, axillary lymph node metastasis significantly increases morbidity and mortality of breast cancer," Etesami said. "Our results show that DBT performs better than 2D mammography alone in what we expect from a screening tool, which is early detection of clinically significant cancers before they spread to axillary lymph nodes."