Breast imaging can be a tricky business. Luckily for ECR 2018 delegates, a slew of experts have provided their top three tips for imaging. You can expect to learn about digital breast tomosynthesis (DBT), automated breast ultrasound (ABUS), and more at today's Special Focus Session.
One of the hottest new technologies in breast imaging is DBT. Evidence continues to mount for the utility of DBT in breast cancer patients. While many argue DBT is ready for "prime time," in other words, breast cancer screening, others are more cautious.
"I believe many countries with population-based service screening are awaiting firmer evidence on, for example, interval cancer rates after screening with DBT," said Dr. Sophia Zackrisson, PhD, an associate professor and senior lecturer in diagnostic radiology at the department of imaging and functional medicine at Skåne University Hospital Malmö at Lund University in Malmö, Sweden. "The challenge is the initial prospective detection trials were not powered for this."
DBT is a popular screening tool, and today she plans to explain how it can be implemented in the near future. She will also touch on artificial intelligence (AI) and deep-learning-based systems, including how they aid in detection and decision-making.
"Computer-aided detection (CAD) for DBT is a necessity, I would say, so I anticipate further studies including CAD," she noted. "Other software tools to aid in the reading of DBT are also of importance."
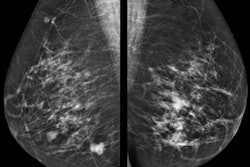
 A 1-cm large tumor in a nondense breast is not evident on digital mammography but is clearly visible on digital breast tomosynthesis. This tumor could easily be missed at digital mammography screening. The case illustrates the fact that not much overlapping tissue is needed to hide a small, spiculated tumor on digital mammography. Images provided by Dr. Sophia Zackrisson.
A 1-cm large tumor in a nondense breast is not evident on digital mammography but is clearly visible on digital breast tomosynthesis. This tumor could easily be missed at digital mammography screening. The case illustrates the fact that not much overlapping tissue is needed to hide a small, spiculated tumor on digital mammography. Images provided by Dr. Sophia Zackrisson.Zackrisson's tips represent a portion of what ECR attendees will learn. The entire session offers a crash course on relevant breast imaging topics, including, for instance, ABUS.
ABUS is primarily designed as a screening tool and has major advantages over handheld ultrasound – other than not dependent on an operator. The technique ensures evaluation of the entire breast in a structured way. Images can be obtained by technicians and read in batch mode by a radiologist. ABUS also enables comparison with prior imaging. It works well for women with dense breasts and provides an overview of the breast, making it useful for extent estimation of larger and more diffuse-growing lesions. However, there are also things to watch out for, such as artifacts, which Dr. Ritse Mann from the radiology department at Radboud University Nijmegen Medical Centre in Nijmegen, the Netherlands, will cover during the session.
ABUS uses a mechanically driven wide-array transducer, which moves over a membrane that compresses the breast, while a woman is imaged in the supine position.
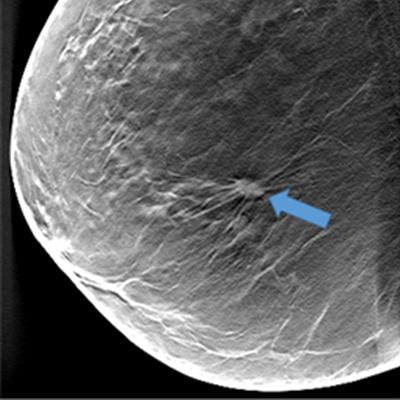
 Lateral ABUS view of the left breast. There is a small, spiculated cancer present in the upper outer quadrant. In the coronal reconstruction (large field), an extensive retraction pattern is seen in the surrounding tissue (yellow arrow). This facilitates quick lesion detection and increases specificity of ABUS reading. Image provided by Dr. Ritse Mann.
Lateral ABUS view of the left breast. There is a small, spiculated cancer present in the upper outer quadrant. In the coronal reconstruction (large field), an extensive retraction pattern is seen in the surrounding tissue (yellow arrow). This facilitates quick lesion detection and increases specificity of ABUS reading. Image provided by Dr. Ritse Mann."A first issue is that skin contact might not always be good, despite the use of a large amount of lotion, leading to reverberation artifacts at locations where air bubbles are caught between the skin and the transducer," he said. "Furthermore, respiration causes a sinusoidal wave in the imaged breast tissue, which might distort, in particular, coronal reconstructions of the image."
The ABUS operator cannot align the transducer head relative to the structures within the breast so quite commonly, Cooper's ligaments are hit tangentially by the ultrasound beam, he added. This causes shadowing artifacts below the ligament that seem to move through the breast.
"We refer to these artifacts as 'wandering shadows.' Similarly, due to suboptimal alignment and a suboptimal focal depth, simple cysts often do not appear completely black, and thus resemble small solid lesions," he said.
Attendees at the session can expect to learn about evaluation of ABUS images, and Mann will speak about caveats that might lead to false-positive and false-negative evaluations.
Axillary staging has important implications for breast workup and will be addressed today.
"The presence of nodal metastases is one of the most important prognostic factors in women with breast cancer," noted Dr. Fleur Kilburn-Toppin, from the radiology department at the Cambridge Breast Unit of Addenbrooke's Hospital in Cambridge, U.K. "It is also important in helping to decide on adjuvant treatment."
Radiologists must be aware of abnormal lymph node morphology, including focal cortical bulge, multilobulated cortex or an absent hilum, and increased cortical thickness, because it will help them determine whether a patient has breast cancer. It's not only breast radiologists who should be on the lookout for these morphologies -- general radiologists may be asked to examine axillary lumps as well.
Kilburn-Toppin will outline how to discriminate between normal and abnormal lymph nodes, when to biopsy, and what the future looks like for this field.
"The future of axillary imaging is rapidly changing with a shift toward less aggressive treatment of the axilla and therefore more importance on radiological imaging," she said. "Better detection of the sentinel node and the ability to discriminate between minimal and advanced nodal disease are important topics of future research."
Also at the session, attendees will learn about complex cystic and solid lesions, contrast-enhanced spectral mammography, various kinds of biopsy, and more.
Originally published in ECR Today on 1 March 2018.
Copyright © 2018 European Society of Radiology