Contrast-enhanced spectral mammography (CESM) is gaining momentum, and like it or not, the technique will be a part of the workup for breast imaging in the future, not least because CESM rivals breast MRI in many ways, according to European breast imaging specialists.
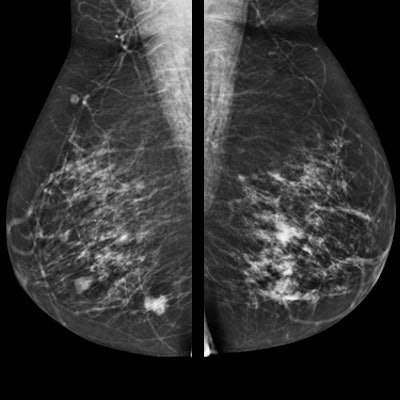
CESM, or contrast-enhanced dual-energy mammography (CEDM), is a mammographic technique in which an iodine-based contrast agent is administered intravenously two minutes prior to image acquisition. In general, an iodine contrast concentration higher than 300 mg/mL is used, with a dose of 1.5 mL/kg body weight. The patient is positioned in the mammography unit like a regular full-field digital mammography (FFDM) examination, with image acquisition consisting of two views per breast: mediolateral oblique and craniocaudal. The procedure uses a low-energy image, similar to FFDM, but it also acquires a high-energy image to visualize iodine uptake.
CESM is generally used in diagnostic settings with clinical indications similar to breast MRI. However, while both CESM and MRI are based on analysis of wash-in and wash-out of breast lesions, several technical differences may influence clinical performance and images interpretation, noted Dr. Clarisse Dromain, PhD, from the imaging department at Lausanne University Hospital in Switzerland, a speaker at Saturday's session. The major differences include 2D versus 3D images, contrast and temporal resolution, type and quantity of contrast agent, acquisition under compression versus free of compression, and positioning, she said.
CESM matches the performance of breast MRI, not only in terms of breast cancer detection, but also in the assessment of disease extent, explained Dr. Marc Lobbes, from the radiology department at Maastricht University Medical Center in the Netherlands. A large, prospective multicenter study conducted wi 178 patients found overall sensitivity of MRI was better than CESM (76% versus 72%), but overall specificity of CESM was better than MRI (94% versus 88%). Furthermore, CESM has fewer false positives than breast MRI, which several studies have confirmed.
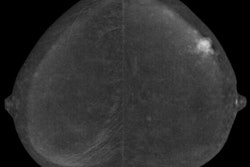
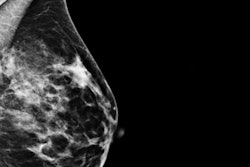
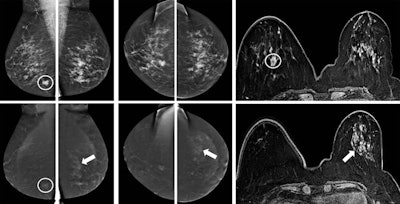 A 57-year-old woman was referred from a private clinic for an ill-defined irregular mass in the right breast, enhancing on both CESM and MRI (circles). CESM also showed diffuse enhancement throughout the left breast, for which random biopsies were taken, showing lobular carcinoma in situ (LCIS). Because of its extent, an MR-guided biopsy was recommended by the multidisciplinary team, again showing LCIS. Based on these findings and the patient's preference, a bilateral mastectomy with reconstruction was performed. Final pathology showed invasive carcinoma of no special type in the right breast, but 10 invasive lobular cancer foci varying from 3 mm to 10 mm in the left breast surrounded by LCIS. Images courtesy of Dr. Marc Lobbes.
A 57-year-old woman was referred from a private clinic for an ill-defined irregular mass in the right breast, enhancing on both CESM and MRI (circles). CESM also showed diffuse enhancement throughout the left breast, for which random biopsies were taken, showing lobular carcinoma in situ (LCIS). Because of its extent, an MR-guided biopsy was recommended by the multidisciplinary team, again showing LCIS. Based on these findings and the patient's preference, a bilateral mastectomy with reconstruction was performed. Final pathology showed invasive carcinoma of no special type in the right breast, but 10 invasive lobular cancer foci varying from 3 mm to 10 mm in the left breast surrounded by LCIS. Images courtesy of Dr. Marc Lobbes."I think it is the combination between your mammographic image (in which you can appreciate the morphology of lesions very well through the high spatial resolution) and the enhancement seen on the recombined images," he told ECR Today. "On MRI, especially with small foci, you see them enhancing, but because of the spatial resolution, it is much more difficult to appreciate the subtle morphology."
Because of CESM's performance, it is already a regular part of the breast workup at Maastricht University Medical Centre and has been since the device's introduction. Radiologists primarily use CESM for recalls from screening but also as a breast MRI alternative, for instance in preoperative staging or response monitoring in breast cancer patients undergoing neoadjuvant chemotherapy. They also use it for unknown primary tumor screening or with highly suspicious findings on a physical exam by the surgeon. The number of annual CESM examinations is, therefore, steadily increasing at the hospital, but CESM will stay a diagnostic tool, and don't expect it to replace mammography screening anytime soon, Lobbes said.
"I think regular mammography is still a very good basic exam," he said. "The proper indications for CESM still need to be figured out in studies, and there are even studies that evaluate whether it could be used for high-risk screening, but I still regard CESM as a sort of 'second-line' mammography study. The use of iodinated contrast agent with potential side effects and the slightly increased radiation dose prevent it from being used in, for example, low-risk asymptomatic women. But we will learn about the indications in the upcoming years, no doubt."
Another area of future interest is whether CESM can replace breast MRI for certain indications. Other questions include whether CESM can be optimized, if less contrast may be used, along with radiation dose, and if the imaging protocol may be optimized. Different timing protocols exist for CT for different indications, so why not for CESM?
"The current protocol is rather robust and works fine, but maybe there is room for squeezing out more details in specialized CESM protocols," Lobbes pointed out.
Joining Dromain and Lobbes at Saturday's session is Dr. Eva Fallenberg from the clinical radiology department at Universitätsmedizin Charité Berlin in Berlin. She will outline the current indications for clinical implementation of CESM and how the modality can be a problem-solver. She will also familiarize attendees with results of published studies on overall performance of CESM compared with digital mammography.
Dromain will discuss the performance of CESM compared with breast MRI regarding lesion morphology and enhancement. She will also present data on the subject.
Originally published in ECR Today on 3 March 2018.
Copyright © 2018 European Society of Radiology