Women with any out-of-pocket expenses for screening mammography are less likely to choose digital breast tomosynthesis (DBT) over digital mammography, compared with women who have complete insurance coverage for the exam, according to a study published online July 24 in the Journal of the American College of Radiology.
Past research has supported this finding, demonstrating that patients who have to pay for mammography are less likely to comply with screening recommendations, wrote a team led by Dr. Emily Sedgwick of Baylor College of Medicine. The new results suggest there's work to be done in communicating to patients that the benefits of DBT merit the extra cost.
 Dr. Emily Sedgwick from Baylor College of Medicine.
Dr. Emily Sedgwick from Baylor College of Medicine."If we are to offer DBT [screening mammography] as an alternative to the gold standard, 2D [screening mammography], it is our obligation to demonstrate that there is a benefit for the additional cost to patients," the authors wrote.
Worth it?
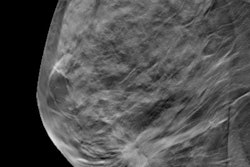
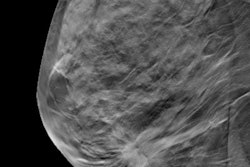
The clinical benefit of DBT has been demonstrated in large studies, and the current study's outcomes fell in line with this research, with reduced recall rates, increased cancer detection, and higher positive predictive values. The researchers' facility transitioned to an all-DBT program in July 2015.
However, insurance coverage is spotty, and this factor appears to contribute to whether women choose to undergo the exam, according to Sedgwick and colleagues.
"In our community, DBT can be found at most breast centers and enjoys prominent local media attention," they wrote. "However, many large payors in our community do not offer 100% payment coverage for patients who choose to undergo DBT screening mammography."
Their study included 9,503 patients who underwent screening mammography between July 2015 and December 2016. Patients were offered a 2D screening mammography and DBT exam or a digital mammography exam at the time of scheduling, at check-in, and before the exam.
The practice's schedulers, front desk staff, and technologists were educated about the risks and benefits of the technology, including a possible co-payment for DBT, so they could pass this information on to patients; the patients were also encouraged to speak with a radiologist if they had questions about which type of exam to choose. In addition, practice radiologists gave talks about DBT versus digital mammography in the community, to practice employees, and to referring physicians.
The patients were divided into three groups: those who had total financial responsibility for any screening mammography, those who had co-payments for DBT, and those who had complete insurance coverage for DBT. Of the total number of patients, 5,079 underwent DBT and 4,424 had digital mammography. DBT produced better results in terms of screening outcomes.
| Screening outcomes for mammography and DBT | ||
| Measure | Digital mammography only | Mammography + DBT |
| Recall rate | 5.4% | 4.4% |
| Cancer detection rate | 3.6/1,000 | 4.9/1,000 |
| Invasive cancers found | 8 | 16 |
| Positive predictive value | 6.7% | 9.5% |
Sedgwick's group found a statistically significant difference between women who chose DBT and those who chose digital mammography, based on their financial responsibility. Among the women wholly responsible for screening exam payment, 48.5% chose DBT over digital mammography; among those who had partial financial responsibility, 39.6% chose the exam. But 70% of women who had complete coverage of DBT for breast cancer screening elected to undergo it.
100% coverage
Because DBT demonstrates better screening outcomes, healthcare providers need to push insurers to cover it, Sedgwick and colleagues concluded.
"In today's era of healthcare value, it is incumbent upon providers to evaluate cost and benefit for the services they offer," they wrote. "On the basis of our correlation of a patient's out-of-pocket expense and underutilization of DBT screening mammography, healthcare providers should advocate that 100% coverage for [the exam] be mandated."