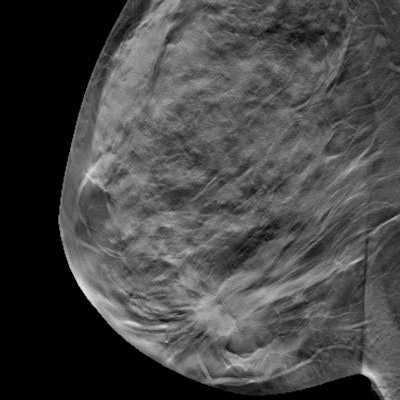
Breast density measurements calculated on full-field digital mammography (FFDM) and digital breast tomosynthesis (DBT) are comparable -- and so are median radiation dose values for dense breasts, according to a study published in the July issue of Academic Radiology.
The findings are further evidence that radiologists can trust DBT for screening patients with dense breast tissue, wrote a team led by Dr. Maria Castillo-Garcia of the Complutense University of Madrid.
"Breast density measurements from both [digital mammography and DBT] lead to equivalent BI-RADS classification ... hence showing no difference in clinical outcomes," wrote the group, adding that "the median mean glandular dose values for dense breasts ... are similar for both FFDM and DBT imaging modalities" (Acad Radiol, July 2017, Vol. 24:7, pp. 802-810).
Cost-benefit analysis
DBT has been shown to find more cancers and reduce recall rates when compared with digital mammography, whether or not a woman has dense tissue, according to the authors. But there has been concern that adding DBT to FFDM increases the radiation dose, a problem that can be exacerbated by dense tissue. To address that issue, some vendors have developed software that synthesizes 2D images from DBT exams, thus reducing the amount of radiation to which women are exposed.
Castillo-Garcia's group sought to compare breast density estimates from two measurement tools on FFDM and DBT and also analyze the impact of individual women's breast density values on mean glandular dose for both modalities. The team included 561 combination FFDM and DBT mammograms taken between November 2015 and January 2016 using Hologic's Selenia Dimensions system with C-View software, which generates synthesized 2D images.
Of the 561 exams, 227 were for women younger than age 50, and 334 were for women age 50 or older. Volumetric breast density was automatically calculated on each modality using Hologic's Quantra 2D and Quantra 3D software. The researchers also analyzed the impact of breast density values on mean glandular radiation dose for both FFDM and DBT.
They found that 71% of breasts imaged were classified under the same category for both modalities, with approximately half in BI-RADS density category C (heterogeneously dense) on both FFDM and DBT density calculations. When compared with the density algorithm for 2D images, DBT had a lower number of breasts in BI-RADS category D (extremely dense), at 43%, and a higher number of breasts in BI-RADS category A (entirely fatty), at 153%, the group found.
As for mean glandular dose, Castillo-Garcia and colleagues found a small increase of 5% or less on DBT in women with extremely dense breasts, but no statistically significant differences between breast density measurements from either of the Quantra algorithms and mean glandular dose.
The study shows that DBT is trustworthy in the screening context, the researchers concluded. In fact, it can replace FFDM -- overcoming that technology's limitations with dense breast tissue.
"According to our results, the small increase of mean glandular dose for women with extremely dense breasts supports the replacement of FFDM by DBT," the group wrote. "The availability of reconstructed 2D mammography from DBT acquisitions facilitates the replacement."