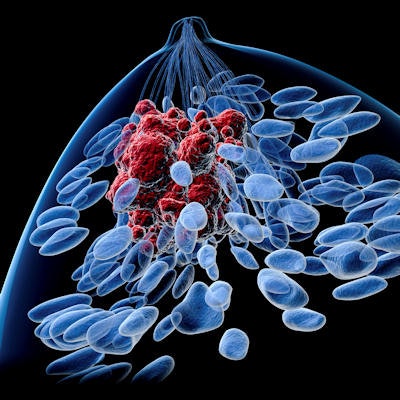
Women at high risk of breast cancer who are undergoing annual breast MRI screening can safely discontinue additional screening mammography, thus reducing their exposure to unnecessary radiation, according to a study published in the October issue of Radiology.
Researchers from Mount Sinai Hospital and Women's College Hospital in Toronto found that among a population of high-risk women, mammography did not detect any cancers that breast MRI missed, and MRI detected three times as many cancers compared to mammography alone.
"Screening breast MR imaging is superior to mammography in detection of invasive and in situ breast cancers," wrote a team led by Glen Lo, who is now at Sir Charles Gairdner Hospital in Perth, Australia. "Our study demonstrated that screening mammography does not improve cancer detection in women who undergo screening breast MR imaging."
Can breast MRI stand alone?
 Glen Lo from Sir Charles Gairdner Hospital.
Glen Lo from Sir Charles Gairdner Hospital.As breast MRI technology advances, its sensitivity over mammography continues to improve in high-risk women, who often have dense tissue as one of their risk factors, Lo and colleagues wrote. And because screening mammography involves radiation exposure, whether it can be discontinued in women undergoing regular breast MRI becomes an important question. So Lo's group sought to evaluate the value of mammography for detecting breast cancer in high-risk women undergoing screening breast MRI (Radiology, October 2017, Vol. 285:1, pp. 36-43).
"I was doing a women's imaging fellowship in Toronto, and my colleagues and I began to notice that mammography was not adding to cancer detection in our patients who were undergoing regular breast MRI," Lo told AuntMinnie.com via email. "We wondered why we needed to perform two screening tests when one would suffice -- especially considering women's concerns about radiation."
The study included 1,977 screening breast MRI scans and 1,957 screening mammograms performed between January 2012 and July 2014 in 1,249 high-risk women. The researchers tracked performance measures such as recall and cancer detection rates, sensitivity, specificity, and PPV1 (the number of cancers found in all exams recalled at screening) for both modalities.
Forty-five cancers were found in 42 women; 33 of the cancers were invasive and 12 were ductal carcinoma in situ. Among the 45 cancers, 29 were identified with breast MRI alone and 14 with both breast MRI and mammography. No cancer was identified by mammography alone, Lo and colleagues wrote.
Further imaging and/or biopsy were recommended in 461 screening breast MRI studies, for a recall rate of 23.3%; further follow-up was recommended in 217 mammography exams, for a recall rate of 11.1%. However, MRI identified three times as many cancers as mammography.
| 2D mammography vs. breast MRI for screening high-risk women | ||
| 2D mammography | Breast MRI | |
| Cancer detection rate (No. of cancers per 1,000 exams) | 7.2 | 21.8 |
| PPV1 | 6.5% | 9.3% |
| Recall rate | 11.1% | 23.3% |
| Sensitivity | 31% | 96% |
| Specificity | 89% | 78% |
In 273 women with a BRCA mutation (mean age, 46), there were 23 cancers, 18 of which were invasive and five of which were DCIS. Breast MRI found 22 of these 23 cancers. In 802 women with at least a 25% estimated lifetime risk of breast cancer (mean age, 44), there were 14 cancers, 10 of which were invasive and four of which were DCIS. Breast MRI found 13 of these 14 cancers.
The fact that mammography was more specific than breast MRI -- and had a lower recall rate -- was not surprising, Lo and colleagues wrote. More breast MRI exams were interpreted as BI-RADS 3 (probably benign, a finding that prompts recall): 180 in all, compared with 16 mammograms in this category.
"As expected, specificity of MR imaging in our study was significantly lower than that of mammography, [although it was] similar to previously reported range (79%-81%) in studies that assigned BI-RADS 3 ... interpretations as positive screening cases," the group wrote. "This is reflected in our higher abnormal interpretation rate of 23.3% for MR imaging versus 11.1% for mammography."
MRI specificity tends to improve when prior comparative studies are available and as readers gain experience, the authors noted.
No need for mammography?
Because mammography did not find any cancers that breast MRI missed, the study results show that it's unnecessary for high-risk women undergoing annual breast MRI screening, Lo and colleagues wrote. This finding should help women as they decide how and when to screen, Lo told AuntMinnie.com.
"We now work in an era of personalized medicine where women are consumers of healthcare," he said. "If a woman younger than 40 at high risk of breast cancer tells me, 'I don't think that mammography is worth the annual radiation when I already do MRI -- and you say the MRI is the most sensitive test,' I can't really argue on the basis of cancer detection alone that mammography adds benefit."
The bottom line is that it's likely safe for women at high risk of breast cancer to be screened only with MRI, the authors wrote.
"We suggest considering using MR imaging as a standalone screening test and diminishing the use of mammography in ... high-risk young women who qualify for annual screening breast MR imaging," they concluded.
Results confirmed
In another study published in the same Radiology issue (pp. 44-52), researchers from the University of Washington in Seattle presented findings that seem to support Lo's. A team led by Dr. Janie Lee investigated breast MRI's interpretive performance in U.S. community practice; her group discovered that it meets or approaches the American College of Radiology's (ACR) BI-RADS benchmarks.
Lee and colleagues used breast MRI data from the Breast Cancer Surveillance Consortium (BCSC). They included 8,387 screening breast MR exams acquired between 2005 and 2013, and linked the data to regional Surveillance, Epidemiology, and End Results (SEER) program and state tumor registries. The group then used BI-RADS benchmarks to assess breast MRI's cancer detection rate, positive predictive value of biopsy recommendation (PPV2), sensitivity, and specificity.
Breast MRI found 17 cancers per 1,000 screening exams; the BI-RADS benchmark is 20 to 30 per 1,000 exams. The modality's PPV2 was 19% (benchmark, 15%), its sensitivity was 81% (benchmark, > 80%), and its specificity was 83% (benchmark, 85%-90%).
"The interpretive performance of screening breast MR imaging in U.S. community practice meets or approaches current BI-RADS benchmarks," Lee and colleagues wrote.




















