What should be done with incidental breast lesions detected in women receiving chest CT exams? A new study recommends not only that these lesions be followed up, but also that a new reporting scale similar to BI-RADS be used to classify the findings, according to results published in Clinical Imaging.
 Dr. Laurie Margolies from Mount Sinai Health System.
Dr. Laurie Margolies from Mount Sinai Health System.
The number of breast cancers found on chest CT is not insignificant, especially when looking at older women, lead author Dr. Laurie Margolies told AuntMinnie.com. Margolies is section chief of breast imaging for the Mount Sinai Health System and a professor of radiology at the Icahn School of Medicine at Mount Sinai in New York City.
"If a chest radiologist reading a chest CT sees something in the breast, it should be reported and acted on, if not already known," she said. "We tried to validate that [process] and developed a system so that radiologists can report the results relatively easily."
Golden opportunity
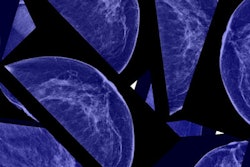
Mammography remains the gold standard for the early detection of breast cancer, and research has shown it to be effective at decreasing mortality. But the recent, albeit slight, decline in mammography usage rates in conjunction with the increasing regularity of chest CT exams has spurred the reporting of breast cancers on CT.
"My great fear is that there will be a group of women who won't have yearly mammograms anymore ... and there is a danger that some of these women will develop cancers," Margolies said. "At the same time, if those women happen also to be getting chest CT exams, whether for lung cancer screening or any other reason, we do have the opportunity to look at the breast [and] see some things on the order of incidental findings."
CT may be the only chest imaging that some women undergo, in which case it provides a chance for radiologists to potentially spot breast nodules that may otherwise go unnoticed, she said. Moreover, evaluating common chest CT scans comes with no additional cost, patient time, or radiation exposure.
Having demonstrated the viability of assessing breast density on chest CT in prior research, Margolies and colleagues compared the reliability of using CT versus mammography for detecting breast masses in the current retrospective study. They began by developing a reporting scale they called the breast assessment and recommendation CT score (BARCS), a nomenclature designed to mirror the BI-RADS standard created by the American College of Radiology (ACR) for reporting screening mammography studies:
- BARCS 0: Incomplete evaluation. A finding on CT scans prompts further evaluation of the breast. This score is analogous to a BI-RADS score of 0.
- BARCS 1: Normal. No abnormality of the breasts is noted. Analogous to BI-RADS 1.
- BARCS 2: Benign findings. Analogous to BI-RADS 2.
- BARCS 6: Known breast cancer. Requires appropriate treatment. Analogous to BI-RADS 6.
CT scans of the women in this retrospective study took place between December 2010 and July 2013 and were for clinical applications other than breast imaging. Each patient also underwent mammography within one year before or after the CT exam.
CT and mammography agree
Two radiologists experienced in mammography and CT independently scored the CT scans of 542 women using the BARCS scale, after first training for uniformity of evaluation techniques on a set of 10 CT scans. The researchers then compared these scores with those previously recorded from the mammograms of the same population following the BI-RADS standard.
Using the BARCS technique, the radiologists found nine invasive cancers on the CT scans -- just shy of the 11 seen on the mammograms. They did not catch any malignant breast cancers on the CT scans that were not also spotted on the corresponding mammograms.
| Mammography vs. CT for breast assessment | ||
| Mammography (BI-RADS) | CT (BARCS) | |
| No. of incomplete evaluations | 96 | 90 |
| No. of breast assessments requiring no immediate action | 436 | 452 |
| No. of invasive cancers detected | 11 | 9 |
Although the radiologists did not catch as many breast cancers on CT as on mammography, it is possible that the two missed cases were not quite as visible on the CT scans as they eventually were when picked up on mammograms four and seven months later.
Comparing their BARCS method with BI-RADS, the researchers found that the two reporting techniques displayed a good to excellent overall percent agreement (77.1%). The agreement was markedly higher among cases that required no immediate action (BI-RADS 1, 2, and 3; 87.6%) than among those that needed further workup (BI-RADS 0, 4, and 5; 34.0%).
Applying the BARCS method is a simple way for radiologists to systematically and accurately assess breast parenchyma for masses on chest CT scans, Margolies said. It provides radiologists with the opportunity to extract important information that may affect a healthcare provider's decisions regarding mammography or other appropriate breast imaging.
The primary limitation of the study was the selection bias stemming from only examining patients who underwent both chest CT and mammography, the researchers noted. These patients may have been more prone to developing cancer than the average population.
Though the researchers continue to report any breast cancers found on chest CT exams, they have not fully integrated the BARCS scale at their institution, according to Margolies. The group hopes to get funding to extend this pilot study in a prospective manner as they prepare to do so.
"A study out of England [by Schramm et al] has already shown that evaluating the breast on chest CT is cost-effective," she said. By looking out for breast cancer on CT scans, "we're not going to be adding a major burden -- either financially or timewise -- to the physician or patient."