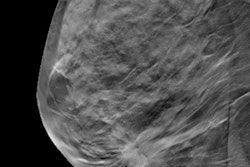
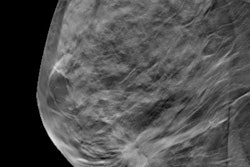
The combination of digital mammography (DM) plus digital breast tomosynthesis (DBT) finds 90% more breast cancer than digital mammography alone -- and with a similar recall rate, according to a study published online June 5 in Radiology.
This higher detection rate could translate into better prognoses for women diagnosed with breast cancer, wrote a team led by Dr. Pierpaolo Pattacini of AUSL Reggio Emilia in Italy. The study is part of the Reggio Emilia tomosynthesis trial (RETomo).
"Tomosynthesis plus digital mammography detects 90% more cancers than digital mammography alone," the group wrote. "This higher detection [rate] may have a beneficial impact on cancer prognosis."
Promising performance
DBT has been shown to be more sensitive than conventional digital mammography in detecting breast cancer, making it a promising technology for screening. But increased sensitivity isn't always a benefit: It can lead to overdiagnosis or an early diagnosis that doesn't change a woman's prognosis, Pattacini and colleagues wrote.
That's why a randomized trial comparing the two modalities is key, according to the group. RETomo is comparing DM plus DBT versus DM alone in screening, and this research is an interim analysis of half the trial's sample size. The analysis included 9,777 women who underwent digital mammography and DBT and 9,783 who had digital mammography alone between March 2014 and March 2016.
The combination of the two modalities found 8.6 cancers per 1,000 cases -- almost twice the rate of digital mammography alone, at 4.5 per 1,000 cases. The recall rate was 3.5% in both the combination and the digital mammography alone groups.
The combination of digital mammography and DBT also found smaller cancers (< 20 mm) and more cancers in dense breast tissue than digital mammography alone. However, it also found more ductal carcinoma in situ (DCIS), the group noted.
| Performance of digital mammography alone vs. DM + DBT | ||
| Measure | DM | DM + DBT |
| Invasive cancers found | 39 | 69 |
| Cancer detection rate per 1,000 cases | 4.5 | 8.6 |
| Positive predictive value (cancers found in total number of recalled women) | 13% | 24.1% |
| Recall rate | 3.5% | 3.5% |
| False positives per 1,000 cases | 30 | 27 |
| Median radiation dose | 4.84 mGy | 11.24 mGy |
| Median read time, negative studies | 34 sec | 56 sec |
| Median read time, recalls | 104 sec | 114 sec |
| Lesion size < 10 mm | 16 | 31 |
| Lesion size ≥ 10 mm to < 20 mm | 14 | 31 |
| DCIS | 5 | 14 |
| Cancers found according to BI-RADS density | ||
| A (fatty) | 2 | 4 |
| B (scattered fibroglandular) | 12 | 25 |
| C (heterogeneously dense) | 18 | 27 |
| D (extremely dense) | 7 | 16 |
The researchers found higher breast cancer detection rates across a variety of measures except for very large or late cancers (those ≥ 20 mm, those at grade 3, and those classified as negative for estrogen and progesterone receptors and positive for human epidermal growth factor receptor 2 [HER2]). These results suggest that the cancers identified with the combination of DM and DBT are the ones clinicians want to find.
"These characteristics, together with the magnitude of gain in detection, suggest that early cancer diagnosis is occurring," the researchers wrote. "This is promising in terms of the impact on prognosis and ultimately on mortality."
But they did note some downsides to using the combination of DM and DBT, including the overdiagnosis of lesions that weren't clinically relevant, as well as longer reading times and higher radiation dose.
"The dose in the experimental arm was 2.3 times higher than that in the control arm," the group wrote. "Using DBT alone could avoid double exposure. In fact, most of the gain in invasive cancer detection observed in the experimental arm was due to DBT alone."
In any case, more research is needed, Pattacini and colleagues concluded.
"Only data on following screening rounds can say to what extent this higher detection rate has an impact on cancer prognosis and reveal the effects of digital breast tomosynthesis on overdiagnosis compared with digital mammography," they wrote.