Breast density advocate Nancy Cappello, PhD, died on November 15 due to complications related to a late-occurring side effect of breast cancer treatment. Cappello was instrumental in passing the first state breast density notification law and in raising awareness of the relationship between breast tissue density and cancer risk.
Cappello died of myelodysplastic syndrome, a type of cancer thought to be related to the aggressive chemotherapy she received years earlier for her original breast cancer. She had been awaiting a bone marrow transplant.
 Nancy Cappello, PhD.
Nancy Cappello, PhD.Cappello was perhaps the single individual most responsible for the growing awareness of breast density as a health risk for women. Prior to her work, the relationship between tissue density and breast cancer was an arcane clinical topic known mostly to researchers and breast care specialists. By the time of her death, it had become a major public health policy concern.
In 2004, Cappello was first diagnosed with stage IIIC breast cancer that had spread to 13 lymph nodes. The 2.5-cm mass was discovered through a clinical breast examination, despite the fact that she for years had received multiple normal mammograms.
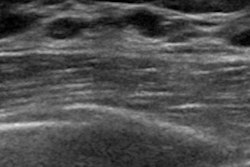
Shortly after her diagnosis, Cappello learned that she had dense breast tissue, which can confound conventional x-ray-based mammography by making it more difficult to visualize abnormalities; however, she had never been told this fact by her healthcare providers. This motivated Cappello to start Are You Dense in 2008 to raise awareness of breast density among women. She told her story in a December 2013 article in the Journal of the American College of Radiology.
One of the group's first initiatives was to pass density notification legislation in Cappello's home state of Connecticut, an effort that was successful in 2009. The law requires women to be notified of their status if they are found to have dense breast tissue on mammograms and to be offered supplemental screening such as ultrasound or breast MRI. The Connecticut law soon led to a "flood" of similar legislation in other states, with dozens passing their own density notification laws.
Many radiologists and breast care providers were originally skeptical of the notification initiatives, seeing them as leading to additional reporting burdens. But many soon changed their opinion as the laws were put into practice and as more knowledge became available about the relationship between dense breast tissue and breast cancer risk.
Most recently, Cappello and other breast density advocates have been pushing the passage of federal legislation that would mandate breast density reporting on a nationwide scale, but a bill has not yet been passed and will expire with the end of the 116th Congress on January 3, 2019. The groups have also been working with the U.S. Food and Drug Administration to change the agency's regulations to standardize breast density reporting across the country.
Over the past year, several studies were published questioning the effectiveness of the state breast density laws, arguing that the legislation wasn't helpful and that it led to higher healthcare costs and even overdiagnosis -- when breast cancers that would never present a threat to a woman's life are worked up and treated.
Cappello and co-authors tackled these concerns head-on in an October 2018 article published in JACR: They found that women in states with breast density laws were more informed about the association between density and breast cancer risk and their own density type. Women from states with density laws also reported that their providers were more likely to talk to them about density, compared with women from states without such laws.
"Our national survey demonstrates that density reporting laws are associated with increased breast density awareness and higher rates of conversations between women and their providers regarding supplemental screening," Cappello and colleagues wrote. "Radiologists and referring clinicians are both involved in engaging women to inform them of their density and risks. Moving forward, patient advocacy groups should advocate for more refined and personalized information about a woman's specific breast tissue category, associated risks, and discussions regarding supplemental screening."