Although the change is modest, supplemental breast imaging and biopsy rates increased in states that passed laws requiring patients to be notified if they have dense breast tissue, according to a study published online May 31 in the Journal of General Internal Medicine.
With respect to supplemental imaging, the findings show that density notification laws are effective if their purpose is to increase screening for women with dense tissue. But there's continued debate about whether supplemental imaging for women with dense breast tissue is effective, wrote a team led by Loren Saulsberry, PhD, of the University of Chicago.
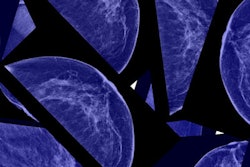
"Dense breast tissue increases breast cancer risk and lowers mammography sensitivity, but the value of supplemental imaging for dense breasts remains uncertain," the group wrote.
Higher breast density has been linked to increased cancer risk, and since 2009, 37 states and Washington, DC, have passed breast tissue density notification laws that require facilities to notify women with dense tissue about this fact and about their supplemental imaging options. But clinical evidence for the efficacy of this approach is lacking, according to Saulsberry's team.
"Prior research suggests that supplemental ultrasonography, MRI, and tomosynthesis may identify additional cancers ... while also increasing false-positive results," the group wrote. "Supplemental breast ultrasounds have been shown to lead to unnecessary biopsies."
To assess the effects of state breast density notification laws on the use of supplemental breast imaging and breast biopsies, Saulsberry and colleagues conducted a study that analyzed supplemental imaging and biopsies before and after the passing of breast density notification laws in 12 states between 2009 and 2014. They compared the findings with 12 matched control states. The group evaluated three time periods related to the density laws: six months before, six to 12 months after, and 12 to 18 months after.
The team found statistically significant increases in supplemental imaging and biopsy after legislation was passed compared with the six-month timeframe before the laws were enacted.
| Impact of density legislation on supplemental imaging and biopsies | ||||
| 6 months before density notification laws | 6-12 months after density notification laws | 12-18 months after density notification laws | p-value | |
| Supplemental imaging rate | 8.5% | 9.4% | 10.1% | p < 0.0001 |
| Biopsy rate | 3.1% | 3.5% | 3.9% | p < 0.0001 |
As for the control states, the researchers found a small increase in the proportion of women with supplemental imaging zero to six months after other states passed density notification laws (9.4%) but an overall decrease over time -- from 8.1% six to 12 months after the laws were passed to 6.8% 12 to 18 months after. For biopsy, control states' rates were lower than legislation states in the six to 12 months and 12 to 18 months following the enactment of breast density notification laws.
The bottom line? These laws raise complicated questions for policymakers, clinicians, and patients.
"As breast density notification laws are implemented, policymakers and clinicians should be aware of the potential effects on care and the cost burden to payers and patients associated with these laws," the team concluded. "More research is needed to understand the effects of these laws on cancer outcomes, including stage at breast cancer diagnosis, potential overdiagnosis of breast cancer, and cancer-related mortality."