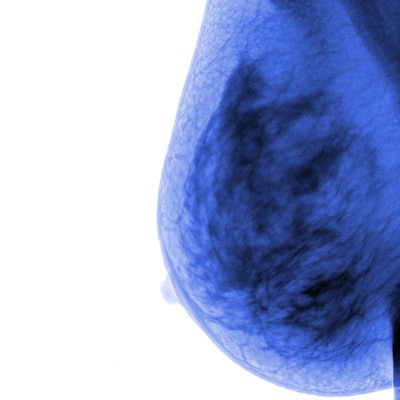
Mammography screening performed annually is the best option for women age 40 to 49, according to a review published online May 15 in the Journal of Breast Imaging. Annual screening is recommended for three main reasons, not least of which is a reduction in breast cancer mortality between 29% and 49%.
And as mammography technology continues to improve, the modality's benefits will also, wrote author Dr. Stephen Feig of the University of California, Irvine.
"Advances in mammography technique and breast ultrasound may allow even better results in the future," he wrote.
Screening mammography guidelines must be crafted according to epidemiologic data such as breast cancer incidence, Feig wrote. A woman's likelihood of developing breast cancer over the next decade increases as she ages. Women at age 40 have a 1.44% chance of developing cancer in the next 10 years; their individual risk is 1 in 69. For women at age 50, the likelihood is 2.39%, with an individual risk of 1 in 42.
"To many observers, these data support beginning screening at age 40 years, rather than age 50 years or later," Feig wrote.
In his review, Feig makes three main points:
- Randomized controlled trials and population-based screening studies underestimate mammography's benefits. "There have been many common limitations in the conduct of virtually all randomized trials and service screening studies that have resulted in underestimates of benefit from screening," he wrote. "These include excessively long intervals between screenings, recall rates that were too low, and biopsy thresholds that were too high. Many studies do not continue screening over a sufficient number of years. Additionally, there have been many successive technical transitions in mammography since these studies were conducted."
- Advances in treatment don't reduce the importance of screening younger women. "There has been a 40% decrease in breast cancer deaths among women of all ages in the U.S. from 1989 to 2016," Feig wrote. "Several mathematical models suggest that earlier detection through screening and advances in chemotherapy, hormonal therapy, radiation therapy, and surgery have all contributed toward reduction in breast cancer mortality. However, modeling provides inaccurate estimates for the relative contributions of screening versus treatment."
- No randomized trial has been designed to compare the relative benefit for different screening intervals for women in their 40s. "Much of the evidence for selection of the best screening frequency for those women is indirect and based on computational models," he wrote. "[But] using data from the National Cancer Institute (NCI) Breast Cancer Surveillance Consortium ... [researchers] found that women ages 40 to 49 years that chose to attend annual mammography were significantly less likely to have node-positive disease than those who attended screenings every other year."
The bottom line? Screening should start at age 40 and continue annually, Feig concluded.
"Annual screening is preferable to less frequent screening, especially during the 40 to 50 decade," he wrote. "Advances in mammography equipment and additional screening ultrasound will allow greater detection sensitivity for younger women with dense breasts."