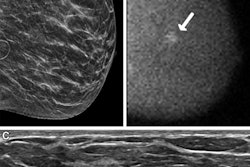
Molecular breast imaging (MBI) is outperformed by mammography in most breast cancer screening scenarios, but it still belongs in the breast cancer screening arsenal, according to a literature review published September 27 in the new journal Radiology: Imaging Cancer.
Mammography is indeed superior to MBI for most breast cancer screening techniques, breast thicknesses, and patient age ranges, reported Drs. Matthew Brown and Matthew Covington, both of the Mallinckrodt Institute of Radiology in St. Louis. However, they also found that MBI actually surpasses the lower range of benefit-to-risk ratios for mammography in some screening scenarios.
"The benefit-to-risk ratios of MBI overlap and, in a few scenarios, exceed the lower range of benefit-to-risk ratios for mammography," the authors wrote. "Use of MBI should, therefore, not be precluded solely on [our study] estimates."
Earlier studies have found the benefit-to-risk ratio for MBI is inferior to that of mammography, but these have been based only on two-view digital mammography, Brown and Covington noted. Yet screening mammography's techniques have expanded to include not only full-field digital mammography (FFDM) alone, but also digital breast tomosynthesis (DBT) plus FFDM, as well as DBT plus synthesized 2D mammography. Radiation dose varies among these approaches, as it also varies according to compressed breast thickness and number of views taken, the team wrote.
Brown and Covington hypothesized the benefit-to-risk ratios for mammography would show wide variation according to technique, breast thickness, and number of views, and that MBI's benefit-to-risk ratio might be equivalent to mammography's in particular scenarios.
The researchers calculated benefit-to-risk ratios as the ratio of breast cancer deaths avoided and lives lost to screening over 10-year intervals starting at age 40 for MBI, FFDM, DBT with FFDM, and DBT with synthetic 2D mammography for two, four, and five views and compressed breast thicknesses of 20 mm to 29 mm, 50 mm to 59 mm, and 80 mm to 89 mm.
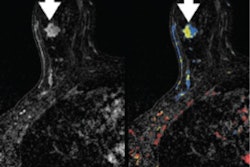
The researchers found MBI's benefit-to-risk ratio was lower than mammography in most of the study scenarios, with the exception of the following -- for which it performed at an equal to or superior ratio: women between the ages of 40 and 69 with a compressed breast thickness of at least 80 mm, and those women undergoing mammography with four or five views per breast.
"On the basis of our results, the maximal net deaths averted occurred in women aged 40 to 69 years; MBI may, therefore, have the most benefit for women in this age range," the researchers concluded. "Because breast density typically decreases with age, women in their first decades of screening are also more likely to be those for whom supplemental screening with MBI may be considered given the presence of dense breast tissue."