With proper training and experience, breast ultrasound consistently improves detection of node-negative invasive cancer in women with dense breasts on mammography, according to a literature review in the Journal of Breast Imaging. Similar results have been observed after digital breast tomosynthesis (DBT).
Thirty-five studies that involved breast ultrasound -- both handheld and automated breast ultrasound (ABUS) -- were reviewed by a team led by Dr. Wendie Berg, PhD, of the University of Pittsburgh School of Medicine, and Dr. Athina Vourtsis, PhD, from the Diagnostic Mammography Medical Diagnostic Imaging Unit in Athens, Greece. They found adding ultrasound to mammography results in low interval cancer rates and boosted cancer detection rates.
"I think it is important that there are now published results on over 400,000 screening breast ultrasound examinations and the results have been very consistent," Berg told AuntMinnie.com. "In women with dense breasts, ultrasound will find another two to three cancers per 1,000 women screened each year."
Why breast ultrasound?
Dense breast tissue can mask breast cancer on mammography, and furthermore, the denser the breast, the greater the risk of developing breast cancer -- a fourfold increased risk, in fact. Dense breasts are so problematic that 38 states as well as Washington, DC, require some form of density information in mammography results letters sent to patients.
In addition, the February 15 federal budget law included a provision that the U.S. Food and Drug Administration (FDA) must update the national Mammography Quality Standards Act (MQSA) to require that breast density is included in mammography reports sent to providers and in results letters sent to patients. The new rule will likely be effective in early 2021.
Considering dense breasts are harder to image on mammography and more likely to conceal breast cancer, what are physicians supposed to do? The answer: Use supplemental ABUS or breast MRI.
The literature review performed by Berg and Vourtsis covered 361,502 exams. Supplemental handheld ultrasound yielded a cancer detection rate of 2.0 cancers per 1,000 women screening, the authors found (JBI, October 31, 2019). For more results, see the table below.
| Performance of breast ultrasound by operator type | |||
| Radiologists using handheld ultrasound | Technologists using handheld ultrasound | ABUS | |
| Cancer detection rate per 1,000 screens | 2.0 | 2.7 | 2.5 |
| Invasive cancers | 87.8% | 86.1% | 91.3% |
| Node-negative cancers | 89.7% | 82.9% | 90% |
Invasive lobular carcinomas averaged 15% to 20% of malignancies in the studies in which the cancers were only seen on screening ultrasound. In nearly all the published studies, the mean invasive cancer size ranged from 7 mm to 13 mm.
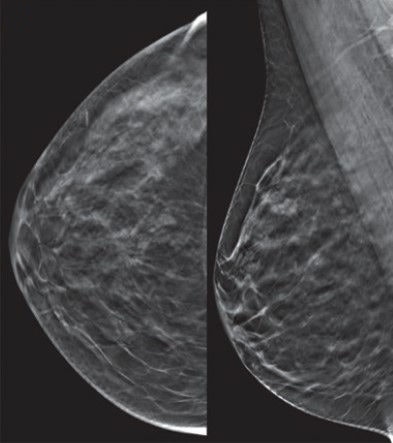 A 50-year-old woman with negative tomosynthesis. Representative craniocaudal and mediolateral oblique 1-mm tomosynthesis images show heterogeneously dense parenchyma in the upper outer quadrant. Two observers (as part of a research study) called this negative, BI-RADS 1. The patient's mother had breast cancer at age 50, as did her maternal great grandfather at age 60. All images courtesy of Dr. Wendie Berg, PhD, and the Journal of Breast Imaging.
A 50-year-old woman with negative tomosynthesis. Representative craniocaudal and mediolateral oblique 1-mm tomosynthesis images show heterogeneously dense parenchyma in the upper outer quadrant. Two observers (as part of a research study) called this negative, BI-RADS 1. The patient's mother had breast cancer at age 50, as did her maternal great grandfather at age 60. All images courtesy of Dr. Wendie Berg, PhD, and the Journal of Breast Imaging.In studies in which technologists conducted the ultrasound, the mean invasive cancer size ranged from 9 mm to 14 mm.
"These are the important cancers to find with screening -- invasive cancers caught early require minimal treatment and have an excellent prognosis, and this is why screening reduces deaths from breast cancer," Berg told AuntMinnie.com. "It is also important that automated screening breast ultrasound showed similar performance."
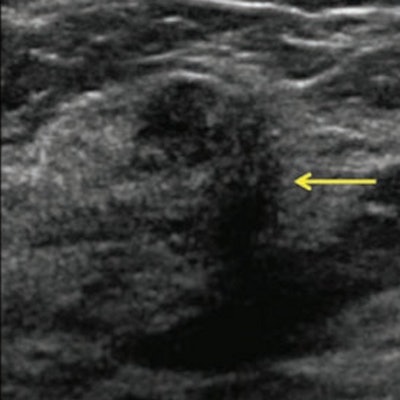
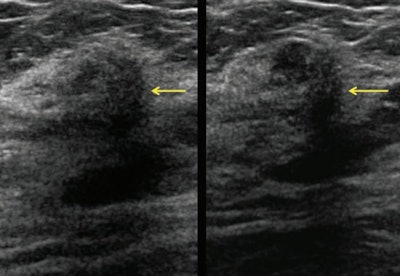 Same patient as above. Screening handheld ultrasound images show this vague indistinctly marginated mass in the right breast at 12 o'clock, 3 cm from the nipple (yellow arrows), assessed as negative by one observer and BI-RADS 4B by the second observer. Ultrasound-guided core biopsy showed invasive lobular carcinoma.
Same patient as above. Screening handheld ultrasound images show this vague indistinctly marginated mass in the right breast at 12 o'clock, 3 cm from the nipple (yellow arrows), assessed as negative by one observer and BI-RADS 4B by the second observer. Ultrasound-guided core biopsy showed invasive lobular carcinoma.In several large studies -- the Japanese Strategic Anti-Cancer Randomized Trial (J-START) and ACRIN 6666 to name two -- ultrasound lowered the rate of interval cancers to a rate similar for women with fatty breasts, she added.
Ultrasound vs. DBT
How does ultrasound fare when it supplements DBT? In the Adjunct Screening with Tomosynthesis or Ultrasound in Mammography-Negative Dense Breasts (ASTOUND)-1 trial, Tagliafico et al reported that when physicians performed ultrasound in 3,231 women, 11 cancers were seen only on ultrasound (an estimated cancer detection rate of 3.4 per 1,000 women). Nearly all cancers (10 out of 11) were invasive with a mean size of 17 mm, and eight out of 10 (80%) were node-negative.
Other studies demonstrated similar results: a cancer detection rate of 2.4 cancers per 1,000 women (Destounis et al, American Roentgen Ray Society, New Orleans: 2017) and 2.6 per 1,000 (ASTOUND-2).
In a mixed screening and diagnostic population of 698 women with dense breasts and 140 cancers, Kim et al (Breast Cancer Research and Treatment, February 2017, Vol. 162:1, pp. 85-94) found that DBT sensitivity was lower than handheld ultrasound sensitivity (91.4% versus 96.4%), but DBT specificity was higher than that of ultrasound (83.9% versus 73.4%).
"Tomosynthesis slightly improves cancer detection compared with standard digital mammography, but there are still some invasive cancers masked by dense tissue even on tomosynthesis," Berg said.
She and her colleagues are conducting a large prospective study of ultrasound after tomosynthesis at multiple centers in western Pennsylvania and will be presenting some of those results at RSNA 2019 in Chicago.



















