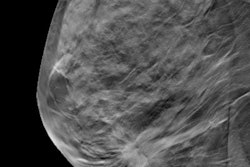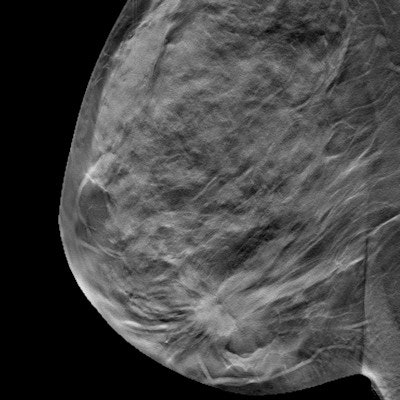
Digital breast tomosynthesis (DBT) is developing fast, but some challenges and questions remain in terms of efficiency, efficacy, safety, and quality assurance, as well as the long-term effect on mortality, two leading researchers have noted in an RSNA 2019 presentation.
DBT is maturing into its role as the technique of choice in mammographic imaging, explained Dr. Yiming Gao and Dr. Samantha Heller, PhD, from New York University School of Medicine, in an e-poster. As of October 2019, national statistics from the U.S. Mammography Quality Standards Act (MQSA) show that almost 65% of all certified facilities and 39% of certified units have DBT capability.
The clinical benefits help to explain this expansion, they noted. For instance, DBT increases the detection of small, node-negative cancers, some of which are DBT-only detected lesions; the average size of DBT-only detected cancers is 8.5 mm (range, 5-21 mm). Also, compared with 2D digital mammography (DM), DBT increases the detection of small, low-grade luminal type and tubular cancers.
"DBT-detected invasive cancers are more indolent and portend better prognosis. On the other hand, it is unclear whether the use of DBT will help improve mortality," the researchers added. "DBT can decrease recall and improve cancer detection, but has not been sufficiently studied to determine if it improves disease-specific mortality."
Industry's contribution
Vendor diversification has helped to speed up the implementation of DBT, but incorporating the technique into clinical-care devices is not always straightforward, they continued. Only four DBT systems currently have approval from the U.S. Food and Drug Administration (FDA), as shown in the table.
| *FDA-approved DBT systems in the U.S. | ||||||||
| Vendor | Tube motion | Scan angle | Projections | Scan time | Detector | Pixel size | s2D | 3D CAD |
| *Hologic Genius | Continuous detector 90° | 15° | 15 | 4 sec | aSe | 100 µ, 70 µ (HD) | *C-view | No |
| *GE SenoClaire | Step/shoot stationary detector | 25° | 9 | 10 sec | a-Si/CsI | 100 µ | *V-preview | Yes |
| *Siemens Mammomat Inspiration | Continuous stationary detector | 50° | 25 | 22 sec | aSe | 85 µ | *Insight-2D | No |
| *Fuji Aspire Cristalle | Continuous stationary detector | 15° (reg), 45° (HR) | 15 | 4 sec (reg), 11 sec (HR) | aSe | 50 µ | No | No |
Even though all commercially available DBT systems achieve geometric accuracies within 0.5%, the systems have different technical and data processing solutions, phantom studies have shown. This leads to notable differences in image quality parameters, including in-plane resolution, geometric accuracy, image noise, and artifact spread function, continued Gao and Heller.
Manufacturers are making technical advances to optimize the examination. For example, the recent development of high-resolution tomography allows significant improvement in overall resolution (smaller pixels), which in turn also improves the resolution of reconstructed 2D synthetic mammograms (SM). This allows better depiction of both masses and more subtle calcifications.
"Compared to conventional SM, SM derived from high-resolution DBT is expected to be able to better depict fine microcalcifications," they stated. "Although there is a trade-off of slightly higher dose for acquisition of high-resolution images, SM in lieu of full-field digital mammography significantly reduces overall radiation dose to the patient. High-resolution imaging has the potential to improve the lower intrinsic resolution of SM, although data are needed to verify this."
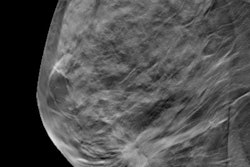
Viewing in slab mode may also help reduce the interpretation time, according to the authors. While DBT studies have consistently demonstrated the benefits of improved sensitivity and specificity as compared to DM, the number of images needed to interpret is many times that of DM studies, especially in cases of large breast volumes.
The picture in Europe
In May 2019, the European Commission Initiative on Breast Cancer (ECIBC) screening guidelines gave a conditional recommendation of DBT for average-risk women between the ages of 45 and 74. Panel members said it is vital to consider how DBT fits within the context of organized screening programs. Cost is a mandatory consideration because resources vary across Europe. Higher radiation dose is another factor, but this is mitigated by synthetic 2D, they pointed out.
DBT is less common in Europe and is not yet the standard of care. It is still primarily used in the context of research in larger centers.
Overall, DBT has highly limited sensitivity in women with extremely dense breasts, and MRI has the highest sensitivity in this subgroup. Also, solitary circumscribed masses on DBT are not always benign and require complete evaluation to exclude the possibility of malignancy.
In the screening setting, DBT has been shown to increase cancer detection and decrease recall. In the diagnostic setting, DBT has been shown to increase BI-RADS1/2 while decreasing BI-RADS 3 categorizations -- in effect, increasing diagnostic confidence.
Latest research findings
Recent global clinical trials have shown the following key points:
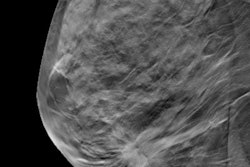
- DBT benefits all age groups across the breast density spectrum, but particularly the 40- to 49-year age group. DBT-detected cancers have a better prognosis than DM-detected cancers.
- DBT with synthetic 2D mammography increases the cancer detection rate as compared to DM, preferentially detecting histologically favorable tumors. The DBT benefit of a lower recall rate may not be seen where the baseline recall rate is already low.
- DBT/DM significantly increases both sensitivity and specificity as compared to DM alone. DBT/SM has similar sensitivity and specificity as DBT/DM in population-based screening, despite the fact that SM has a lower spatial resolution than DM.
- DBT improves the cancer detection rate to a greater extent in Europe, where biennial screening is the norm, and reduces the recall rate to a greater extent in the U.S., where baseline recall rates are relatively high. This confirms that a technology's effects are significantly influenced by differences in clinical environments.
- Longer-term data are not yet available, but existing data suggest that the benefit of DBT in increasing cancer detection and decreasing recall rates appears to be sustainable over multiple rounds of screening.
With the clinical end goal of mortality benefit in mind, the biological profiles of screen-detected breast cancers have become increasingly important, the authors pointed out. Trials are now underway to better understand cancer yield from DBT (anatomic imaging) versus MRI (functional imaging) to determine how best to detect the most relevant cancers in terms of improving mortality.