Vacuum-assisted image-guided breast biopsy can reliably predict which breast cancer patients treated with chemotherapy have responded well enough that follow-up surgery is not required to remove residual cancer, according to a December 13 presentation at the 2019 San Antonio Breast Cancer Symposium (SABCS).
The multicenter clinical trial led by Dr. Henry Kuerer, PhD, a professor of breast surgical oncology at the University of Texas MD Anderson Cancer Center in Houston, found a special protocol for certain breast cancer patients based on image-guided vacuum-assisted biopsy produced a negative predictive value (NPV) of 97.4% and an overall accuracy of 89.5% in determining which ones had residual cancer.
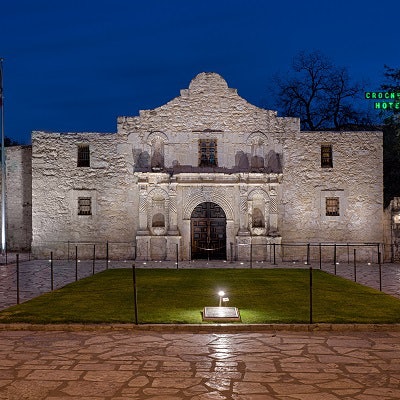
 Dr. Henry Kuerer, PhD.
Dr. Henry Kuerer, PhD.After undergoing neoadjuvant chemotherapy for breast cancer, is the disease truly gone, with no need for follow-up surgery? Clinicians are increasingly turning to image-guided biopsy of the tumor bed to detect residual disease and determine if some women can be spared from undergoing surgery.
In a presentation at SABCS 2019, the question was examined by a research group led by Kuerer that included patient data not only from the U.S. but also the Royal Marsden Hospital in London and Seoul National University Hospital in South Korea.
The trial included 166 women who underwent image-guided biopsy of the tumor bed after neoadjuvant chemotherapy. The majority (n = 143) underwent vacuum-assisted biopsy, while 23 had core-cut biopsy, with six biopsy samples acquired. Most women (n = 129) had an ultrasound-guided biopsy and the others had a stereo-guided biopsy. The majority of the women (n = 160) had invasive ductal carcinoma (IDC). The median tumor size pretreatment was 33.5 mm.
In all, 51.2% of the women in the study showed pathologic complete response to chemotherapy -- meaning no residual cancer. When image-guided biopsy was used, researchers found a false-negative rate of 18.7% for determining residual cancer across the entire study population.
But the group was able to reduce the false-negative rate to 3.2% with a protocol that used vacuum-assisted biopsy on particular patients who are the most likely to respond well to neoadjuvant chemotherapy. One group is those with residual abnormalities 2 cm or smaller and who were positive for human epidermal growth factor receptor 2. In this group, the protocol had a false-negative rate of 3.2%, a negative predictive value (NPV) of 97.4%, and an overall accuracy of 89.5%.
Similarly good results were found for women with triple-negative breast cancer, also known to be good responders to chemotherapy. In this subgroup, vacuum-assisted biopsy produced a false-negative rate of 4.2%, an NPV of 97.2%, and an overall accuracy of 87.9%.
The researchers concluded that their protocol -- image-guided vacuum-assisted biopsy of tumor beds measuring up to 2 cm with at least six samples in women likely to be pathologic complete responders after chemotherapy -- was a good tool for finding women most likely to not need surgery.
"This data shows that through image-guided vacuum-assisted biopsies on patients who achieve a complete pathologic response to chemotherapy, accurate predictions of residual disease can be made, opening the door for potential avoidance of surgery," Kuerer said. "This would be a major step toward improving quality of life for patients with breast cancer."



















