The benefits of digital breast tomosynthesis (DBT) stand the test of time, according to a five-year retrospective study published on March 10 in Radiology. The study found DBT had better cancer detection and fewer false positives than digital mammography throughout multiple screening appointments.
This was one of the first studies to evaluate DBT beyond an initial breast screening session -- when cancer detection and recall rates are likely to be higher. Lead author Dr. Emily Conant attributed DBT's continued success to its ability to create a simulated 3D visualization of breast tissue.
"As a radiologist, tomosynthesis allows viewing of the breast in multiple layers or slices," said Conant, a professor and chief of breast imaging at the University of Pennsylvania Perelman School of Medicine, in a press release. "This ability to scroll through slices of otherwise overlapping breast tissue helps us not only detect more cancers but also better characterize benign or normal areas of the breast."
Better cancer detection, lower recall rates
Few long-term studies have looked at the cancer detection and recall rates of DBT after more than one screening round, the authors noted. In addition, the few studies that have looked at these rates over time hadn't found any significant changes -- until now.
For their study, the authors included women ages 40 or older who underwent preventive breast screening at a University of Pennsylvania hospital in Philadelphia between 2010 and 2016. At the outset of the study, all 29,310 participants had no symptoms or personal history of breast cancer.
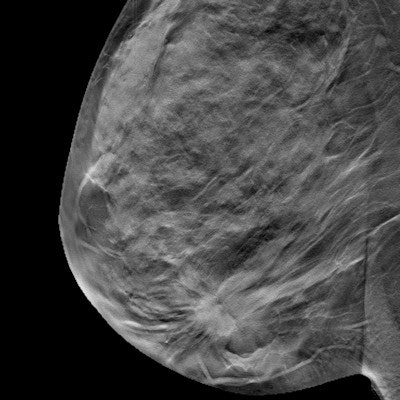
The authors then compared cancers found through the 10,511 digital mammography scans and 56,839 DBT scans included in the study to cancer cases reported in the Pennsylvania cancer registry.
| 5-year performance of mammography vs. DBT | ||
| Digital mammography | Digital breast tomosynthesis | |
| Cancers per 1,000 scans | 5 | 6 |
| Recall rate | 10.4% | 8% |
| Invasive cancer sensitivity | 80.4% | 89.8% |
Over the five-year study, DBT detected more cancers with a lower recall rate than digital mammography. DBT also detected a higher proportion of invasive cancers than digital mammography,
Furthermore, the two modalities performed about the same for false-negative results and biopsy recommendations. The rates also generally held steady throughout the five years of the study.
"We showed that the improved performance with DBT was maintained over multiple years," Conant said. "This is the longest follow-up with cancer registry matching that has been published thus far."
Importance of diverse participants
The study benefitted having from a diverse group of participants, the authors noted. For instance, about half of the study group were African American women, a population at a greater risk of aggressive breast cancer.
"We found different types of biology in the cancers detected across our diverse population, and that's an important takeaway of this paper," Conant stated. "Our results show that we can improve our screening outcomes for younger women with DBT by finding clinically important cancers earlier with fewer false positives."
While the findings demonstrate that DBT appears to be a promising modality for breast cancer screening, the authors noted more studies with similarly diverse populations and even longer follow-up times are needed to confirm the results.
"This is very promising and important data that certainly can be used to model larger trials," Conant said.