Artificial intelligence (AI) image analysis software developer Lunit is touting results from two recent studies that found its Insight MMG software was as accurate as an average radiologist at identifying breast cancer from mammograms.
In an August 24 study in the Lancet Digital Health, researchers found that Lunit Insight MMG could potentially cut radiologist reading time by more than half without impacting cancer detection. Similarly, an August 27 study in JAMA Oncology showed the algorithm was more accurate than first-reader radiologists for detecting cancer from mammograms.
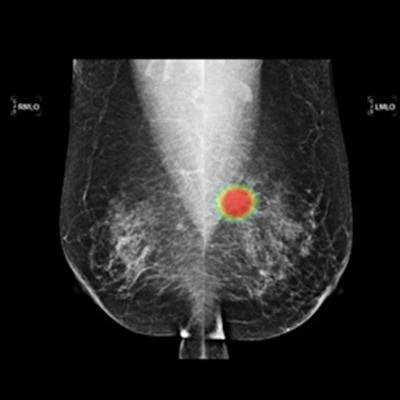
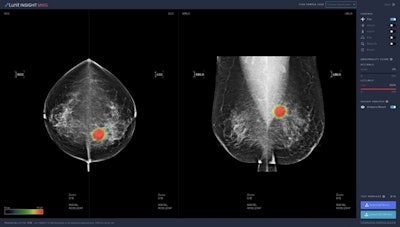 Lunit's Insight MMG AI software for breast cancer detection. Image courtesy of Lunit.
Lunit's Insight MMG AI software for breast cancer detection. Image courtesy of Lunit.Lunit's AI algorithm generates a numerical score that represents the likelihood of a particular mammogram showing cancer. Higher scores from the software equate to greater suspicion of cancer.
In the Lancet Digital Health study, the authors hypothesized that Lunit's score could be used to filter out mammograms from women at low suspicion of having cancer, freeing radiologists up to focus on more suspicious images.
The results proved their hypothesis correct. When Lunit's AI algorithm filtered out mammograms with the lowest 60% of scores, the software did not miss any cancers that would have been otherwise detected by radiologists.
The authors also used the program to identify women with the highest risk of cancer who could potentially benefit from additional MRI screening. When the program selected women with the top 1% of AI scores for additional screening, it could have detected 24 additional interval cancers and 48 screen-detected cancers. When expanded to women with the top 5% of scores, the program could have detected an additional 53 interval cancers and 121 screen-detected cancers.
Lunit Insight MMG showed similar strength in the JAMA Oncology study, which compared the performance of radiologists and three different AI programs for detecting cancer from more than 8,000 mammograms.
The Lunit program achieved a sensitivity of 81.9%, higher than the other two programs evaluated in the study as well as first-reader radiologists (77.4%) and second-reader radiologists (80.1%).
The results were even stronger when the first-reader radiologist results were combined with AI. This combination yielded a sensitivity of 88.6% and specificity of 93%. In fact, combining first-readers with AI identified more positive cancer cases than the joint efforts of two radiologists.