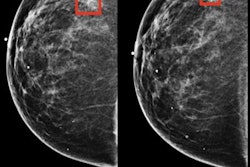
Artificial intelligence (AI) software could help cut down on the number of interval breast cancers, according to research presented Monday at the 2020 virtual RSNA meeting. An AI program detected more than one-third of breast cancers missed on screening mammography in two different studies.
While breast screening programs can reduce the number of breast cancer deaths, many cancers still go undetected on screening. Researchers, including those at the RSNA, are looking into AI as a tool to help prevent these interval cancers.
"About half of these we can see in the previous screening round, so they are missed by the radiologists," said one presenter, Dr. Ritse Maarten Mann, PhD, from Radboud University Medical and the Netherlands Cancer Institute in Amsterdam. "The question is can we improve upon this? Can artificial intelligence help?"
The answer appears to be yes, according to the two studies presented at a breast imaging AI session. In his study, Mann and colleagues found ScreenPoint Medical's Transpara AI software could more accurately predict short-term cancer development than breast density.
The study included 2,332 mammograms of consecutively diagnosed interval breast cancers between 2011 and 2015 as well as the prior screening mammogram. It also included 4,664 control cases matched by age and year at diagnosis.
An analysis of the top 10% of cases flagged by the AI program for having the highest risk for cancer produced a sensitivity of 37% and an area under the curve (AUC) of 0.73. In comparison, cases with the top 10% of breast density had an AUC of 0.70 and sensitivity of 23%.
While the AI program was more accurate than breast density, Mann said they are different but complementary screening tools.
"AI shows you the cancers that you can see on the mammo," he said. "Whereas if you do something else for women with very dense breasts, you might find cancers that are just not visible on mammography."
Mann's presentation was complemented by one from the U.K. that found the same AI program identified 21% of interval cancers on prior mammography screening. The research was presented by Dr. Sarah Jane Vinnicombe, the lead consultant radiologist and honorary senior lecturer at Thirlestaine Breast Centre, Cheltenham, U.K.
Vinnicombe and colleagues analyzed 300 consecutive interval cancers diagnosed between 2011 and 2016. They also included 853 controls who were slightly younger and had lower breast density.
The researchers first set the AI program to screen only the top 4% of mammograms with the highest cancer risk. At this threshold, the program correctly flagged 19% of false-negative cases on a prior screening mammogram as well as 9% of cases with true interval cancers that couldn't at all be seen on prior mammography.
However, the number of detected cancers doubled when the researchers set the program to screen the top 10% of mammograms with the highest cancer risk -- the same percentage used by the Dutch research team. At this threshold, the program flagged 39% of false-negative cases and 21% of true interval cancers.
"We find it interesting that AI-based [computer-aided detection (CAD)] yielded high global scores in nearly one-fifth of all true interval cancers at 90% specificity," Vinnicombe said. "So perhaps this is a group that might require enhanced screening."
Based on their findings, both Mann and Vinnicombe reached the same conclusion: AI can visualize at least some interval cancers missed by radiologists on screening exams.
"AI does have the potential to reduce interval cancers," Mann said. "As a preselection tool, it could determine which women could benefit from additional evaluation."